Article:
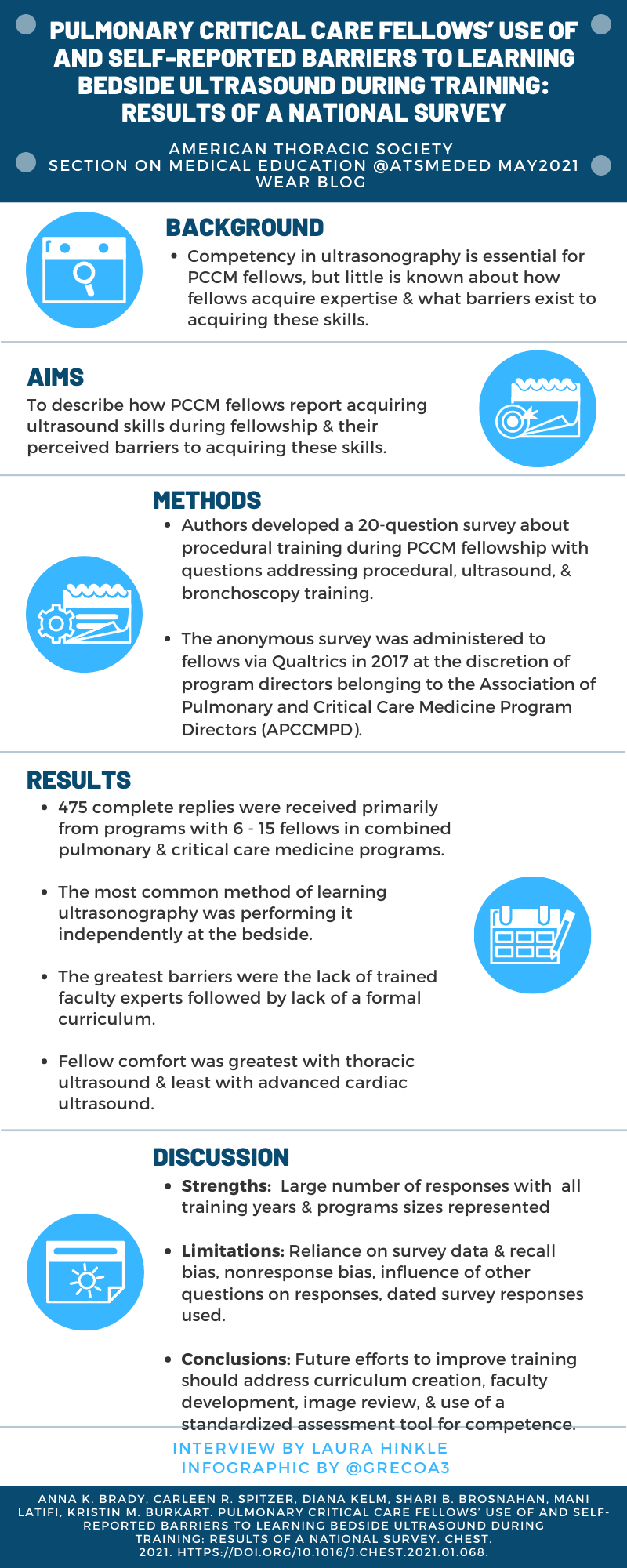
Pulmonary Critical Care Fellows' Use of and Self-reported Barriers to Learning Bedside Ultrasound During Training: Results of a National Survey.
Brady, A. K., Spitzer, C. R., Kelm, D., Brosnahan, S. B., Latifi, M., & Burkart, K. M. (2021). Pulmonary Critical Care Fellows' Use of and Self-reported Barriers to Learning Bedside Ultrasound During Training: Results of a National Survey. Chest. doi:10.1016/j.chest.2021.01.068
Summary:
Ultrasonography is widely recognized as an important skill for critical care physicians. In this study, Dr. Brady, et. al. sought to understand the comfort level of pulmonary and critical care medicine fellows in performing bedside ultrasound exams, how they learned ultrasound skills, and what barriers they experienced to achieving competence in ultrasonography. A total of 475 fellows responded to the survey. Respondents indicated greater comfort in performing thoracic (92%) and focused cardiac (76%) exams than for vascular ultrasound (51%), FAST (46%), or advanced cardiac (22%) exams. Independent learning at the beside was the most common way fellows reported learning ultrasonography followed by formal didactics and simulation. Only a quarter of respondents reported reviewing images with expert faculty. The main barriers to ultrasound training were identified as lack of formal curriculum, limited faculty expertise, and lack of time for image review and training. These last two are the most problematic as they directly conflict with recommendations from expert ultrasound educators that emphasize mentoring and review of images by experts as essential components of ultrasound education. These areas along with development of standardized tools to assess ultrasound competency were identified as domains to target to ensure the next generation of intensivists achieve competence in this vital skill.
Interview:
LH: You were in your final year of training when you initially had the idea for this project. What was it that initially sparked your interest in studying this?
AKB: I was working with a group of fellows from across the country, through the Association of Pulmonary Critical Care Medicine Program Directors (APCCMPD). I had noticed that while at first blush, there seemed to be a lot of ultrasound education for PCCM fellows out there, the lived experience of us as fellows – at a lot of different programs – was that ultrasound teaching actually seemed pretty variable. We suspected that the uptake of ultrasound curricula and teaching wasn’t as uniform as it seemed - we thought it was probably more robust at some places and less so at others, but we didn’t know if our perception was accurate on a large scale, so we wanted to study it. The ultrasound questions were actually part of a larger survey about procedural training in fellowship in general, but when we got the results we thought the ultrasound answers were most interesting to share with the PCCM education community.
LH: Based on discussions with fellowship program directors, do you find that they share the fellows’ opinions regarding existing barriers, or do they identify different roadblocks?
AKB: As I alluded to, this project arose out of fellows having a different perspective – which I try to keep in mind now that I’m a faculty member! Since I’ve become an associate program director myself, I’ve definitely talked about this issue with other fellowship directors. The lack of faculty expertise and the lack of faculty time are common themes. Often there will be one or two champions at an institution, but these faculty may be champions for other educational issues, too, and everyone’s time is so limited. Also, curricula that require one person to do all the teaching are doomed, in my opinion, so lacking widespread faculty expertise is a big barrier – you need a deep bench, so to speak, not just one champion. I think fellowship educators have a lot of competing demands, which I appreciate more now as a faculty member myself.
LH: Your point that faculty expertise needs to increase in order to train our fellows to be competent in critical care ultrasonography is spot on. If this is not addressed, the problem of graduating trainees who lack confidence in their skills will continue to be perpetuated with each generation of pulmonary and critical care medicine physicians. What do you think is the best way to address deficiency in faculty skills?
AKB: I think overconfidence in ultrasound skills – whether it’s image interpretation or knowing when NOT to rely on bedside ultrasound – is just as big of a risk of the problem of lack of faculty expertise. I’m not sure there’s one best way to solve this challenge. I think interdisciplinary education is one possibility to improve education for fellows and faculty. At my institution, we’ve started to take advantage of ultrasound experts in internal medicine and anesthesiology in addition to PCCM to teach our fellows, but we can definitely improve, and I’d love to see faculty learn from each other, too. Programs could pay for faculty to attend national courses to get the basics, but for anyone who is a novice or even intermediate (faculty or fellow) I think large didactic offerings are probably necessary but not sufficient to create the expertise truly needed. It’s really doing a lot of exams and integrating the data in clinical practice that’s needed, and that work takes a lot of time and effort.
LH: What do you see as the next steps in raising the bar for ultrasound training and evaluation of competency in pulmonary and critical care fellowship training?
AKB: I’d love to see more well-designed educational tools that could be used at least to teach ultrasound content, for starters (physics, knobology, evidence for and against using bedside ultrasound in different scenarios). More assessment tools with validity evidence would be hugely helpful, too. I’d also love to see interdisciplinary and even inter-program collaboration for image review.
LH: What advice would you give to current trainees who want to get involved in medical education research like this? Where should they start?
AKB: If you don’t have medical education research mentors at your current institution (or even if you do!) I recommend getting involved with one of the national societies – ATS, CHEST, or APCCMPD, for instance. Within ATS, the Section on Medical Education has often set up ways to facilitate connections between medical education researchers over the years. Even just casual connections from a conference can be ways to launch projects. I’ve participated in multi-institution research projects that came out of a casual coffee meeting at ATS and others that were through a more formal group from the ATS SoME, or – in the case of the ultrasound project, the APCCMPD.
Blog post author

Laura Hinkle, MD completed her nursing degree at Indiana University and practiced for 7 years prior to beginning medical school. She completed medical school, internal medicine residency, chief residency, and pulmonary and critical care fellowship at the Indiana University School of Medicine. She is currently enrolled in in the University of Cincinnati Master of Education degree program and serves as an Assistant Professor of Clinical Medicine in the Division of Pulmonary, Critical Care, Sleep, & Occupational Medicine at Indiana University. Her education related roles are Associate Program Director for the Pulmonary and Critical Care Fellowship, Key Clinical Educator, and Director of Transitions Curriculum. Dr. Hinkle has been actively involved in the American Thoracic Society since she was a trainee and currently serves on the Executive Committee of the Section on Medical Education and leads the Section’s Interprofessional Education Scholarly Working Group Pod. Her scholarly education interests are curriculum development and evaluation.
Twitter: @LauraHinkle18
Article author

Anna K. Brady, MD completed her undergraduate studies at Case Western Reserve University and medical school at the Cleveland Clinic Lerner College of Medicine, followed by residency in internal medicine at the Hospital of the University of Pennsylvania. She moved to the Pacific Northwest for pulmonary and critical care fellowship at the University of Washington, where she also completed the Teaching Scholars Program. She is now an Assistant Professor in the Division of Pulmonary and Critical Care Medicine at Oregon Health and Science University in Portland, OR. At OHSU she is an associate program director for the PCCM fellowship, serves as core faculty for the internal medicine residency, and is active in medical school education as well. She serves on the American Thoracic Society's Section on Medical Education Executive Committee, as well as the ATS Training Committee, where she has been heavily involved in the Innovations in Fellowship Education program and the ATS Resident Bootcamp. Her scholarly interests within education include procedural teaching and curriculum evaluation.
Twitter: @AKBradyMD