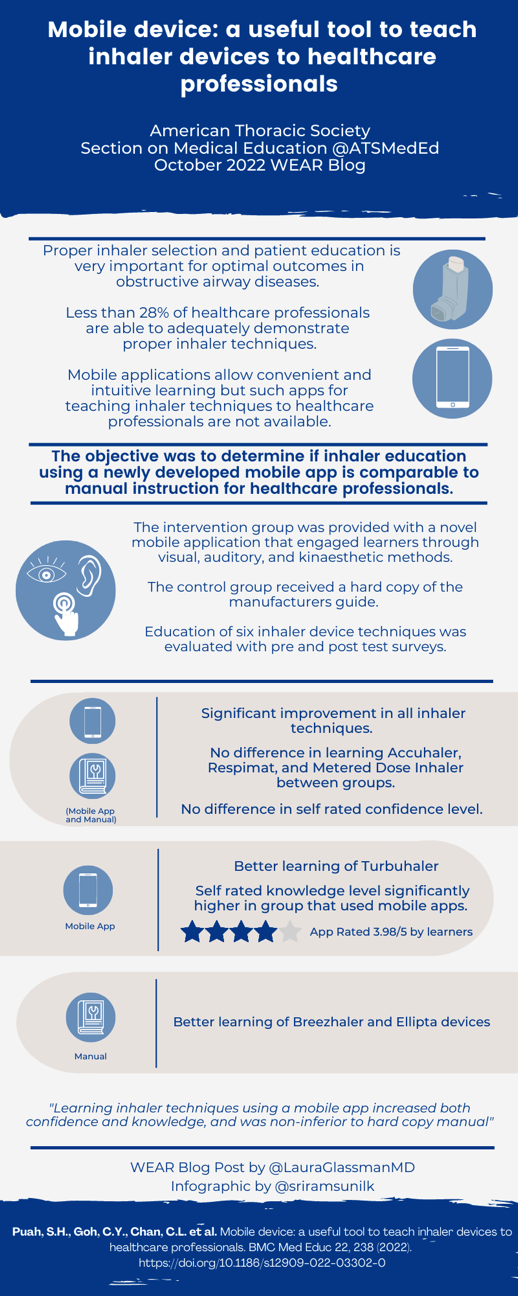
Mobile Device: A Useful Tool to Teach Inhaler Devices to Healthcare Professionals
Citation: Puah, S. H., Goh, C. Y., Chan, C. L., Teoh, A. K. J., Zhang, H., Shen, Z., & Neo, L. P. (2022). Mobile device: a useful tool to teach inhaler devices to healthcare professionals. BMC medical education, 22(1), 1-8.
Summary
Correct inhaler use is crucial in controlling many respiratory diseases, yet most healthcare providers (HCP) often exhibit incorrect inhaler technique, impacting their ability to teach their patients. In this study, the authors designed an interactive mobile application to teach proper techniques for common inhalers. This app utilized visual, auditory, and kinetic feedback by mimicking the user's actions on the screen: including playing a rattling noise when the phone was shaken mimicking the inhaler, and using the phone's microphone to provide feedback on the length of the user's inhalation. HCP were randomized to undergo inhaler training by either using the app or reading the manufacturer's instruction guide. Both groups underwent pre and post-intervention evaluation and overall significantly improved their inhaler technique. The experimental group performed better on the Turbuhaler, while the control group performed better on the Ellipta and Breezhaler. Interestingly, both groups had difficulty demonstrating correct use with the MDI inhaler, despite being one of the most common types of inhaler. Most experimental group members found the mobile app to be a valuable teaching tool and felt they would continue to revisit the app over time.
Interview
LG: Studies have shown that few Healthcare Providers (HCP) are able to correctly demonstrate proper inhaler technique. What factors do you think contribute to such low proficiency in inhaler technique among HCW?
SHP: My personal opinion is that although we prescribe and we counsel for the correct and appropriate use of the inhalers, most of us have not used these inhalers ourselves, hence the lost of contextuality or personal experience. When I first tried the inhalers on the app, I realized I was sucking in too hard and that was bad technique and it made the team understand now how some patients are inhaling the dry powdered inhalers. Just like any procedure that require some form of hand-eye coordination, and in this case hand-eye-mouth coordination, some practice will be required.
LG: Do you envision this application being available to patients as well? If not, what specific information did you include in this application specifically for HCPs?
SHP: The main purpose of the app was for education purposes. We included the drug formulary and information into the app to help with information sharing but the use of the mobile app itself is not limited to healthcare professionals. Our team was hoping that this will be the new way of educating healthcare professionals and patients.
LG: The app has many unique and advanced features such as using the microphone to capture the sound of inhaling and mimicking shaking the phone to the inhaler on screen. How did you come up with these interactive features?
SHP: It was a team effort and it was the co-created together between the medical team consisting of a doctor, the respiratory nursing clinicians and the engineers in Nanyang Technology University who were the brilliant group of people who managed to capitalize on the advancing technology on our mobile phones. The phone's gyroscope sensors were used to mimic the shaking of the inhaler, its touch screen functions allow us to mimic removing of caps and pressing down on buttons while the sound waves recorded were used to match flow rates. There were many discussions on how to make this be as close to the actual inhaler usage as possible and based on the results, we managed to demonstrate very similar correct steps when compared to the manufacturer's instructions.
LG: Why do you think technique for MDIs rated poorly among both groups? What changes to the application would you make to improve the teaching of this very common inhaler?
SHP: I think the MDI requires one of the most coordination between steps. This is likely the reason why the technique was rated to be poor. As the session was only conducted over a short period of time, I think that it will get better with practice. To answer your question, prior to showing competency for the MDI, the learner will likely have to undergo a few practice sessions under supervision for direct observation and feedback. One thing I would like to add into the app is the usage of MDI via an Aerochamber as this is common practice for us to prescribe patient's their technique remains poor.
LG: Do you have plans to implement a similar type of interactive app for other education topics? Is there one Pulmonary/Respiratory topic you have in mind?
SHP: At this juncture, there are no other plans in the works for inhalers. We are currently in the midst of a research on post COVID19 physiotherapy using a mobile app to help with rehabilitation from home with the help of our physiotherapists. This was designed hoping to get patients home early and assist them in home rehabilitation to prevent long COVID symptoms.
Blog Post Author
Laura Glassman, MD, is a second year pulmonary and critical care medicine fellow at University of California, Los Angeles. She completed her internal medicine residency and chief resident year at UCLA. Her clinical interests include airway disease and smoking-related lung disease. She is also passionate about medical education and curriculum development.
Twitter: @LauraGlassmanMD
Article Author

Dr Puah Ser Hon, is a Consultant in the Department of Respiratory and Critical Care Medicine, Tan Tock Seng Hospital, Singapore. He graduated from the International Medical University with an MBBS in 2004 and obtained his MRCP (UK) in 2010. He completed his advance training in respiratory medicine in 2015 and intensive care in 2017. He is a fellow of the Royal College of Physicians and Surgeons (Edinburgh) and a Fellow of the Academy of Medicine of Singapore, in both the Chapter of Respiratory Medicine and Chapter of Intensive Care Medicine.
Dr Puah has a keen interest in medical education and is an avid educator. He is involved in both undergraduate and postgraduate education and is currently pursuing a Masters in Healthcare Professionals Education from Maastricht University. He has won multiple teaching awards. He was honoured with the Dean's Award for Teaching Excellence in 2019 and the National University of Singapore Medicine Special Recognition Award in 2020 from the Yong Loo Lin School of Medicine, National University of Singapore. He also received the National Health Group Teaching Excellence Award – Special Commendation Award in 2020. He is Adjunct Senior Lecturer with the Lee Kong Chian School of Medicine, National Technology University, Singapore, and a Clinical Lecturer at the Yong Loo Lin School of Medicine, National University of Singapore. He is currently the Programme Director for the National Health Group Respiratory Medicine Residency Programme.
Outside education work, he is currently the Clinical Director for the Respiratory Therapy Services and is currently Chair of Tan Tock Seng Hospital's Smoking Cessation Workgroup. He is also involved in research in both the field of respiratory and critical care medicine and has various publications in both fields.
Twitter: @Ser_Hon