Article:
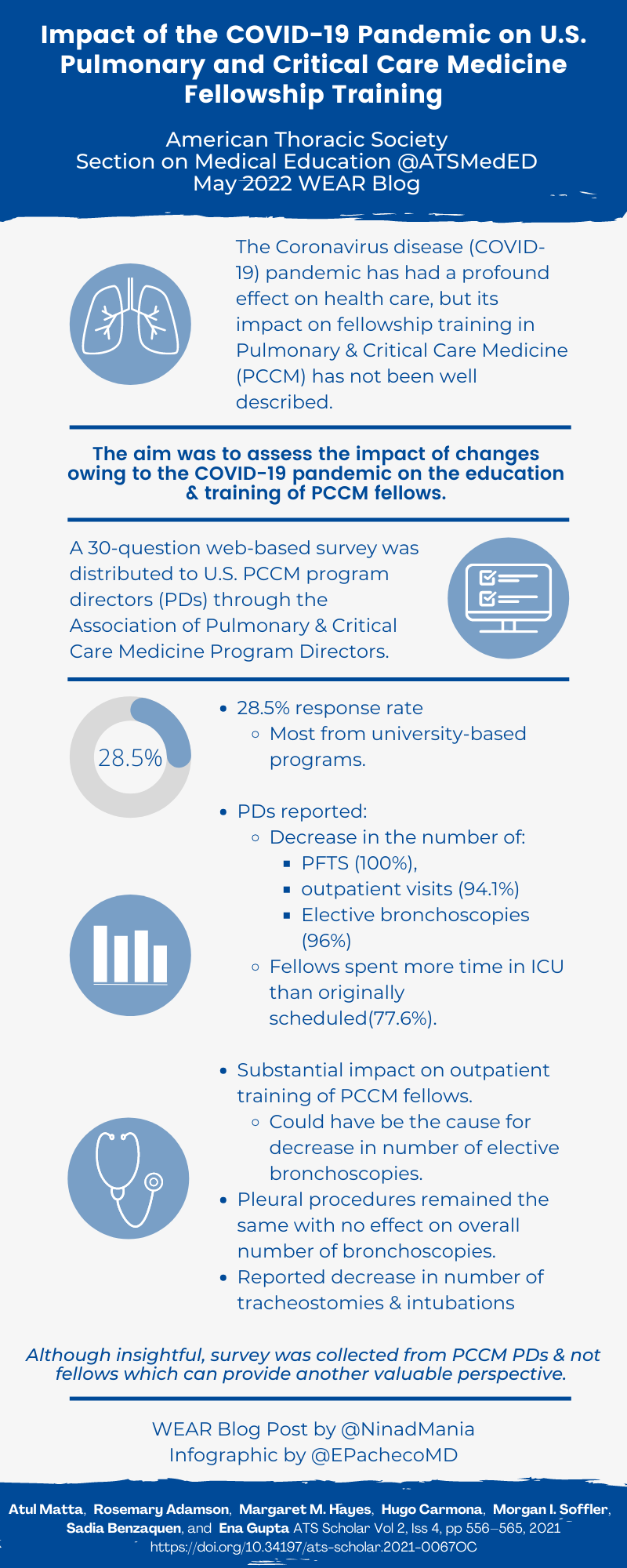
Impact of the COVID-19 Pandemic on U.S. Pulmonary and Critical Care Medicine Fellowship Training
Matta, Adamson, Hayes, et al.: Impact of the COVID-19 Pandemic on PCCM Training. ATS Scholar Vol 2, Iss 4, pp 556–565, 2021
Summary:
The COVID-19 pandemic has posed a unique set of challenges to those within the pulmonary and critical care medicine (PCCM) community. Specifically, the pandemic has led to changes in the composition of clinical training for PCCM fellows. This article explores these changes and their impact based on survey responses from program directors (PDs) of PCCM fellowships across the US. Program directors reported a decrease in the number of pulmonary function tests and elective bronchoscopies at their institutions. The majority of PDs also reported an increase in the proportion of clinical time spent in the Intensive Care Unit (ICU). PDs also reported a decrease in the number of ICU bronchoscopies, intubations and tracheostomies. Overall, PDs felt that the impact of the COVID-19 pandemic on PCCM training was variable or negative with only a minority reporting no impact. Some limitations include a low response rate to the survey, university-based programs being overrepresented and inclusion of PCCM-only fellowship programs. Regardless, this important paper is one of the first to assess impact of the pandemic on PCCM fellowship training and highlights the need for further research based on trainee perspectives and for planning mitigation strategies to minimize the negative impact of the pandemic on PCCM training.
Interview:
NM: What do you think would have been the outcome of this survey if the fellows in training had responded rather than the program directors?
EG: It would be very interesting to design a survey for pulmonary and critical care fellows. I suspect their personal experience might vary depending on their level of training during the pandemic. The decrease in the number of outpatient bronchoscopies might significantly affect the learning curve of new fellows. The experience in the ICU would be perceived differently as well ranging from a robust experience with respiratory failure, ARDS, certain ICU procedures to exhaustion and burnout. It would be very important to capture emotional and psychological well-being among pulmonary critical care fellows and how it will affect them in their future going forward.
NM: Interesting to note an increase in in-house attending staffing during the pandemic. Why do you think this happened?
EG: In my opinion, increase in in-house attending coverage reflects increase in workload. For example, there was an increase the number of ICU teams or ICU attendings at any given time as there was a significant increase in the ICU census during the pandemic. Already heavily burdened ICUs with limited ability to increase staffing during surge likely experienced significant strain including exhaustion of the healthcare workforce. While SCCM does not recommend a particular patient to intensivist ratio, they recommend frequent reevaluation of staffing. Now more than ever we need to carefully think about how thin we want to stretch the healthcare workforce. A durable system is the one with tensile strength to stretch during unforeseen circumstances. Rigidity leads to breakdown in the face of adversity. We need measures to support the healthcare workers with resources and have mechanisms to increase staffing on demand.
NM: Do you think the decrease in the number of bronchoscopies can be mitigated by simulation? Perhaps the pandemic can improve our focus on higher quality simulation that not only improves technical detail but also situational training which for PCCM is often a crucial variable.
EG: I do think there is a role for stimulation in training and assessment of bronchoscopy skills. It a useful tool to practice basic and advanced bronchoscopy skills in a safe and well controlled environment. It will provide a cushion for changes in number of bronchoscopies performed with changes in the future.
NM: Do you think that in the new era of COVID-19 with vaccination and greater ease of obtaining PCR including rapid tests, that elective bronchoscopy numbers will return to baseline?
EG: Yes absolutely, I think that elective will return/have returned to baseline.
NM: What is the next most important aspect of study as a follow-up to the results of this study?
EG: There are several important aspects that deserve further evaluation. For example, a focused group discussion with the program directors to formulate recommendations for preparedness to prevent impact of any future crisis on pulmonary critical care fellow. Also, it is essential to study burnout among pulmonary critical care physicians and trainees so we can better understand it prevalence, its impact and ways to prevent burnout amongst trainees.
Blog Post Author
Ninad Maniar, MD
George Washington University
Twitter: @ninadmaniar
Article Author
Ena Gupta, MD
Albert Einstein Medical Center
Twitter: @enagupta_pccm