Article:
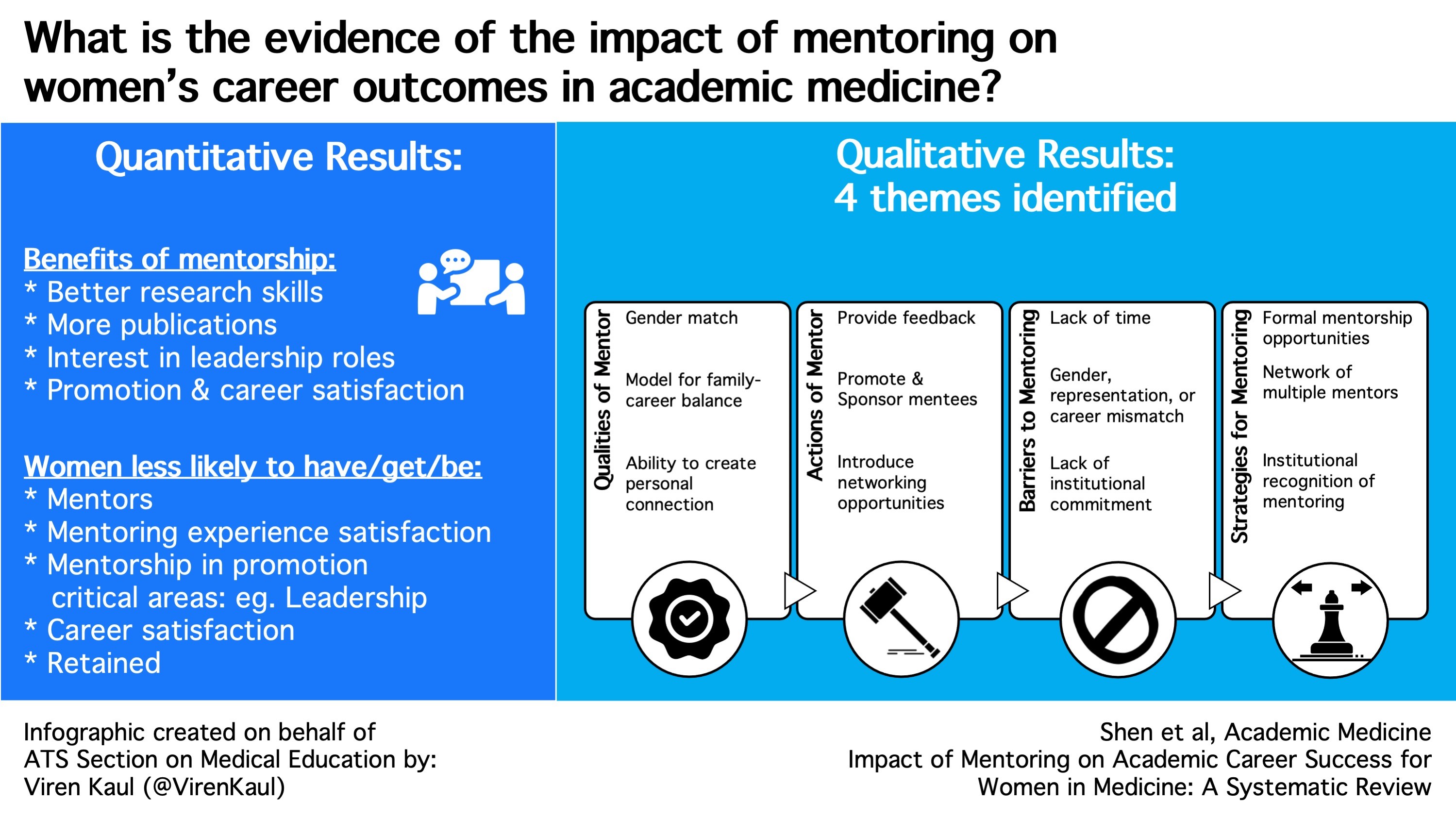
Impact of Mentoring on Academic Career Success for Women in Medicine: A System Review
Shen M, Tzioumis E, Andersen E et al. Impact of Mentoring on Academic Career Success for Women in Medicine: A Systematic Review. Academic Medicine. 2022;97(3):444-458. doi:10.1097/acm.0000000000004563
Summary:
Despite increased representation of individuals identifying as women (hereafter referred to as women) in medical school graduates, numerous reports continue to indicate underrepresentation of women in senior academic leadership positions. Research has shown that barriers to career success in academic medicine disproportionately affect women, including inadequate mentoring, which may perpetuate this underrepresentation. Dr.Shen and colleagues performed a systematic review to examine the impact of mentoring on women's career outcomes and to inform future interventions to support the promotion and retention of women in academic medicine. There were 91 studies examined, inclusive of both qualitative and quantitative data on mentoring and spanning multiple countries over three decades. Overall, women were likely to perceive mentorship as valuable to their career development but were equally likely to report a scarcity of mentoring. This was shown to have detrimental effects on career advancement and satisfaction, in addition to research productivity. Gender disparities in medicine continue to exist but perhaps with studies such as this one we can identify existing barriers, allowing for increased awareness and subsequent solutions.
Interview:
HC: Was there a personal impetus to this study?
MS: This study stemmed from a faculty development session led by co-authors, Dr. Susan Girdler and Dr. Erin Malloy that I happened to attend as a medical student. I was surprised to find out about the "leaky pipeline" in academia, which led us to pursue this work.
In fact, while we all know mentoring is important, there had never been a systematic review demonstrating that mentoring can actually help with improving retention and success for women in academic medicine. Our goal was to establish a baseline of literature to inform future interventions and policies on a departmental and institutional level.
My personal experiences reflected some of the findings in the paper, specifically that women in academic medicine place more importance on mentoring, but have more difficulty finding mentors. Finally, as the majority of the authors of this study are female, despite coming from various backgrounds, we collectively had a passion for bringing this study to fruition.
HC: As a surgeon, you are in a procedurally based field whereas our readers span the spectrum. In your analysis of current literature for the study, did you find any studies analyzing the differences in mentoring in procedural versus non-procedurally based fields?
MS: We did not specifically look at differences in mentoring procedural versus non-procedurally based fields as it was outside the scope of our study. However, it would be a thought-provoking next area of study, given that a lot of procedural-based specialties are male-dominated (e.g., surgery, interventional cardiology, interventional radiology). Our systematic review found that female mentors were noted to be important, especially in male-dominated fields. However, there certainly needs to be more research in this domain.
HC: Having analyzed such a large contingent of studies, do you feel there are any early measures departments without formalized mentoring programs should take?
MS: To support women in academic medicine, even early measures could be impactful. First, solely the recognition and understanding by colleagues and administration that women have added obstacles in finding mentorship is important. Secondly, departments can create recognition and compensation for mentoring contributions in the form of mentoring awards and incorporating mentorship into the promotion packet. Finally, supporting formal mentorship for women (regardless of the gender of mentor) through pre-arranged mentorship, peer mentoring opportunities, and networking events would be essential.
HC: Any plans for changes in mentoring within your home institution and department as a result of this study?
MS: We are fortunate that we actually have several venues for mentorship at the University of Michigan, ranging from the Michigan Women's Surgical Collaborative, the Women in Surgery interest group, and the Association of Women Surgeons chapter. The administration has been incredibly encouraging of efforts to fund and support formal mentoring groups as a result of this work for female medical students, residents, and junior/mid-career faculty.
HC: Finally, any future areas of research related to this topic?
MS: Next areas of research for this topic will include exploring the role of mentoring in academic medicine for women experiencing intersections among social, economic, and political disadvantage. Furthermore, aiming to gain the perspective of women in academic medicine who have experienced structural barriers to mentorship and advancement such as race, sexual identity/orientation, age, and disability via mixed methods research. It would also be important to further work that examines departmental and institutional efforts to further mentoring, rather than individual efforts.
Blog Post Author

Christiana Hayward, MD is a second pulmonary critical care medicine fellow at the University of California Los Angeles. Clinical interests include drug induced pulmonary diseases, though she has a burgeoning interest in asthma. Her medical education interests focus on curriculum development, specifically the optimization of trainee learning within the intensive care unit setting.
Twitter: @HeyDrHay_Ward
Article Author

Mary R. Shen, MD MSc is a fourth-year general surgery resident at the University of Michigan. Her academic interests include social determinants of surgical health outcomes and advocating for diversity, equity, and inclusion in medicine.
Twitter: @mary_shen