Article:
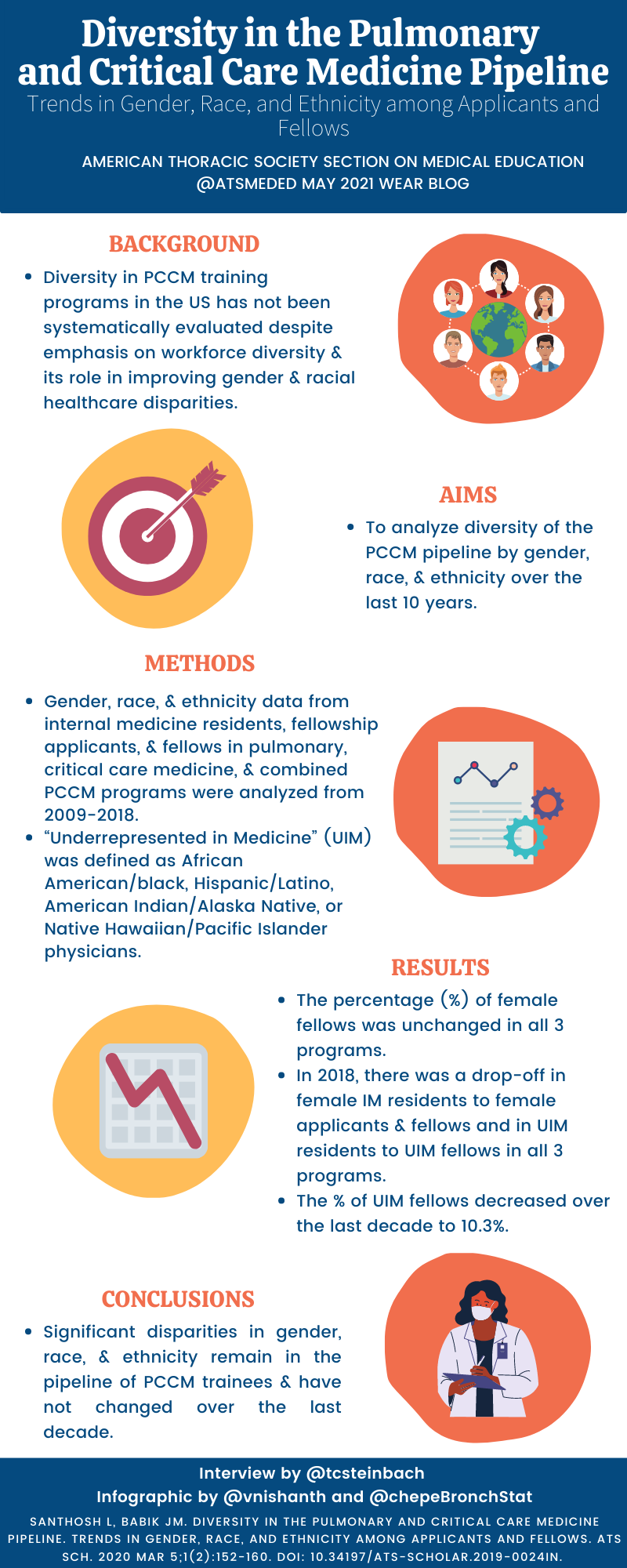
Diversity in the Pulmonary and Critical Care Medicine Pipeline. Trends in Gender, Race, and Ethnicity among Applicants and Fellows.
Lekshmi Santhosh and Jennifer M. Babik (2020). Diversity in the Pulmonary and Critical Care Medicine Pipeline. Trends in Gender, Race, and Ethnicity among Applicants and Fellows, ATS Scholar, 1:152-160.
Summary:
Drs. Santhosh and Babik analyzed the pipeline from Internal Medicine (IM) residency into Pulmonary and Critical Care Medicine (PCCM) fellowships in the United States, characterizing trends in gender, race, and ethnicity over the last decade. They examined demographics at each step of the pathway, including IM residency, fellowship applicants, and matched fellows using data from the GME census and ERAS. They demonstrated that despite an increasing number of total residents in IM, the percentage of women and underrepresented minorities has trended downward. In PCCM specifically, they discovered a large drop off from the percentage of women and underrepresented minorities between IM residency and applicants for fellowship, suggesting an urgent need to nurture a more diverse training pool. Their findings highlight that the PCCM workforce does not reflect of the diversity of the US population. While the article does not examine data for undergraduate medical education, the findings also highlight that the PCCM workforce is not reflective of the diversity within contemporary medical school students. They offer several suggestions to begin addressing this “leaky” pipeline into PCCM.
Interview:
TS: Your paper is vitally important as we work to make our profession reflect the demographics of the patients we serve, what prompted you to look specifically at the pipeline into PCCM specialties?
LS: Thanks so much, Dr. Steinbach for reading this article! Initially, I was inspired by this question at our own institution. I wondered, ‘Are there gender and race/ethnicity differences in residents going into various subspecialties at UCSF? How have these trends changed over time?’ Finding out the answer to this question led me to want to explore these trends more deeply at a national level, so my mentor and I worked to collect national data to answer these questions for all subspecialties, and to drill down on our own field of PCCM.
TS: Your analysis highlights the fellowship application step as a key point in the “leaky” pipeline for women and under-represented in medicine (UIM) in PCCM careers. Do you think there is a systematic feature of our specialty that dissuades these applicants from applying to our field?
LS: We have many hypotheses, and I have a follow-up study to test these hypotheses with further qualitative analysis of UIM residents through focus groups. Our specialty has traditionally been more male-dominated, with significant room to improve with both gender and racial/ethnic diversity. Concepts of stereotype threat, impostor syndrome, and lack of role models may play an important role in this. Moreover, we cannot deny that the effects of systemic racism and sexism play a role in medical education at all levels. We have to actively combat the stereotype of a “bro culture” in PCCM and work to make our specialty more inclusive and welcoming to all.
TS: The other interesting (and alarming) data your work identified is the declining proportion of IM residents who are women and UIM; why do you think this is occurring despite growing diversity in undergraduate medical education? Are we moving backwards? Furthermore, what immediate steps can all PCCM faculty (not just those in leadership or education) take now to increase diversity within our training pool and workforce?
It is concerning that over time, the percentage of UIM trainees was unchanged in IM residents. This outlines the fact that diversity, equity and inclusion are not a ‘fellowship’ or ‘faculty’ problem, they are systemic problems at all levels which require systemic changes.
Dr. Quinn Capers is a national scholar on this topic and he outlined some important recommendations in his piece in ATS Scholar, “How Clinicians and Educators Can Mitigate Implicit Bias in Patient Care and Candidate Selection in Medical Education.” I agree with these key recommendations – that we should remove photos from ERAS applications and de-emphasize biased metrics like USMLE scores, train selection committee members on implicit bias and how to reduce bias, adopt a holistic review approach in fellow selection, and work to recruit and retain UIM students, residents, fellows, and faculty at every level. This is just a starting place for programs, and I hope that all programs will take Dr. Capers’ sage advice in operationalizing these recommendations.
Blog Post Author

Trevor Steinbach, MD is an Assistant Professor at the University of Colorado in the Division of Pulmonary Sciences and Critical Care Medicine. He serves as the director for the pulmonary fellows clinic and the APD for Ambulatory Education in the Pulmonary and Critical Care Fellowship program. His academic interests include curriculum design, leadership education, and ambulatory pulmonary curricula.
Twitter: @tcsteinbach
Article Author

Lekshmi Santhosh, MD, MAEd is an Assistant Professor of Pulmonary/Critical Care Medicine and Hospital Medicine at the University of California-San Francisco (UCSF). She is the Associate Program Director of the Pulmonary/Critical Care Medicine Fellowship program. Her scholarly interests focus on transitions of care, women in leadership, and clinical reasoning.
Twitter: @LekshmiMD