Article:
Characteristics of Effective Teachers of Invasive Bedside Procedures: A Multi-institutional Qualitative Study. Chest. 2020 Nov;158(5):2047-2057. doi: 10.1016/j.chest.2020.04.060. Epub 2020 May 16
Diana J Kelm, Jennifer L Ridgeway, John T Ratelle, Adam P Sawatsky, Andrew J Halvorsen, Alexander S Niven, Anna Brady, Margaret M Hayes, Jakob I McSparron, Kannan Ramar, Thomas J Beckman.
Summary:
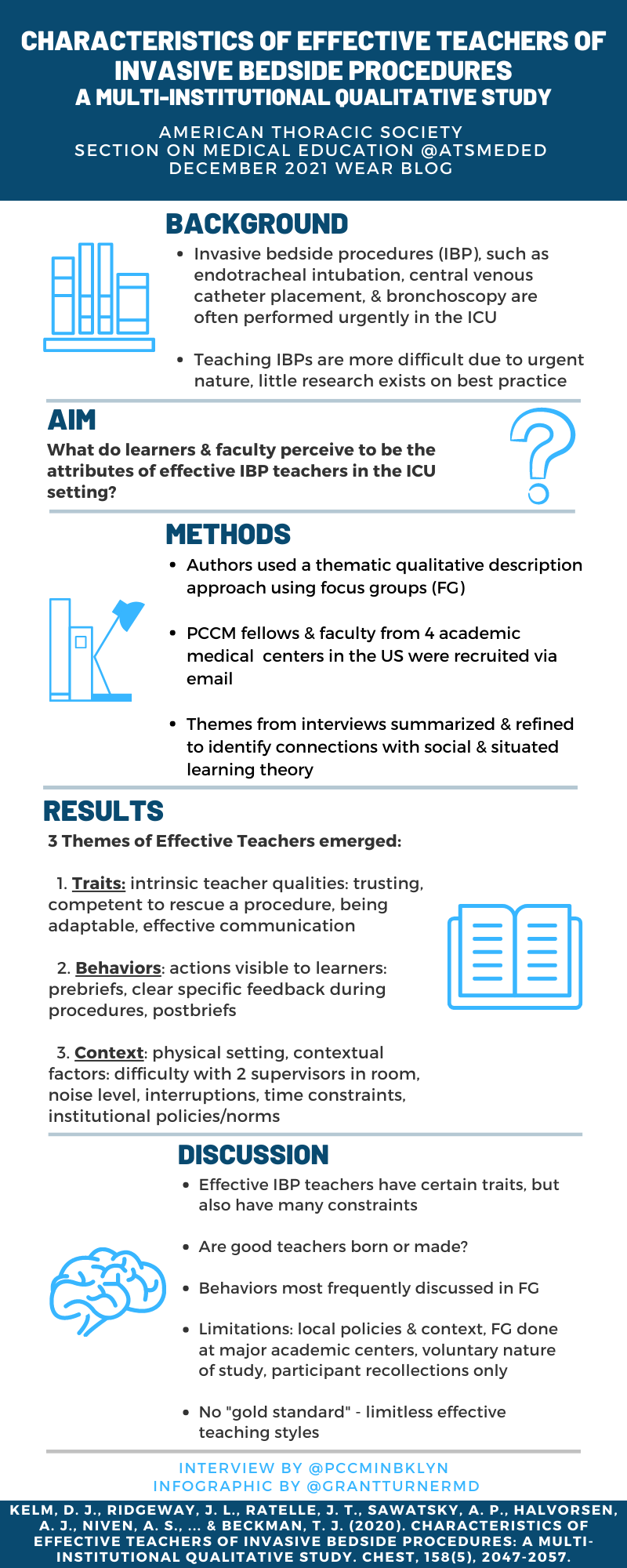
A variety of invasive procedures are performed at bedside in the intensive care unit, often under urgent or emergent conditions. Technical errors can lead to procedural complications with resultant adverse events for patients. Trainees can improve their procedural skills with supervision by more experienced operators, but prior research on what makes for an effective teacher of invasive bedside procedures (IBPs) has been limited to settings that do not include the ICU, and may not be generalizable to the needs of ICU learners, teachers and patients.
Kelm et al. conducted focus groups (FGs) of pulmonary-critical care medicine (PCCM) fellows and attendings at four academic medical centers in the US, in order to identify characteristics of effective IBP teachers by learning from the experiences of these learners and teachers. Using a thematic qualitative description approach, informed by constructs from social and situated learning theories, the investigators identified specific categories of themes related to characteristics of effective IBP teachers. A total of 30 fellows and 33 faculty participated in FG sessions with a median duration of 49 and 54 minutes, respectively. Three themes related to the characteristics of effective IBP teachers were identified by the investigators: (1) traits, (2) behaviors, and (3) context. Behaviors were the most frequently discussed characteristic of effective IBP teachers among both fellows and faculty, for example pre-procedure briefings and post-procedure debriefings/feedback. This qualitative study’s findings can inform further investigation of effective IBP teaching by observing teachers and learners in real-time to confirm the characteristics noted by FG participants. The authors note that while some traits of effective IBP teachers are in-born, PCCM faculty development sessions that aim to educate teachers on the behaviors discussed in this study may be an effective means of improving on the quality of IBP teaching in the ICU.
Interview:
MA: Your article notes prior work done on the teaching of invasive procedures, but that there is a relative paucity of data specific to teaching in the ICU. What is different about teaching bedside procedures in the ICU versus other clinical contexts, and what are some of the unique challenges faced by attendings and learners in the ICU when it comes to procedural training?
DJK: Teaching bedside procedures in the ICU is different from teaching procedures in other clinical settings for a few reasons. The most common issue is time – we never have enough of this! Although this isn’t unique to the ICU, the main challenge we face is that the procedures we perform in the ICU often occur on an urgent/emergent basis, which limits our time to think and forces our hands to act quickly. In addition, we also have limited time to discuss the procedure with the trainee. One of the biggest discussion points during our focus groups was the importance of a pre-brief which involves a discussion before the procedure, which includes understanding the learner’s prior experiences, discussing roles and expectations, and learner assessment to help the teacher adjust their teaching strategy. Due to varying ICU schedules, teachers may not have the time and prior experiences to build an educational rapport with a learner. If a teacher has worked with a learner before, the dynamics may be different depending on that prior experience. Lastly, the patients in the ICU are critically ill, often with hemodynamic instability and/or respiratory failure on top of their usual co-morbidities. We need to be both competent with the procedure and efficient as the patient could clinically decompensate during the procedure. This often puts pressure on the teachers and may affect the learner’s autonomy and opportunities for procedural teaching.
MA: For readers not well versed in qualitative research methods, what are some of the most notable differences from the quantitative methods with which many of us are more familiar from our medical education?
DJK: Both are important but have different methodologies and outcomes. Quantitative studies focus on the numbers and statistics. The results tend to be black and white. The interpretation of the results includes statistical analysis. On the other hand, qualitative studies involve stories with an emphasis on the words and the meaning behind those words. The results can be quite gray and harder to analyze. The best way to interpret these results would be in the lens of theoretical framework to allow useful interpretation and analysis of the results.
MA: How do you and your co-authors define the three categories of themes that were identified as related to the characteristics of effective IBP teachers: traits, behaviors, and context?
DJK: Traits are the intrinsic characteristics of the teacher. Behaviors represent the things that the teacher does or the actions that are visible to the learner. Context includes the environment, institutional cultures or policies, and patient-specific factors that influence teaching effectiveness.
We noted an interesting intersection between these themes which may affect the procedural teacher’s effectiveness. For example, a teacher can be anxious (trait) about supervising a procedure with a new learner. They may display anxiety with specific behaviors that are visible to the learners such as tapping their feet, speaking fast, or using a harsh tone. The context of the environment may be enhancing the teacher’s anxiety, such as the patient is hemodynamically unstable, and they have clinic in 60 minutes.
MA: What would you recommend to educators and pulmonary-critical care training program leaders that are looking to apply lessons learned from this study to their efforts to improve on bedside procedural education at their institutions?
DJK: Although effective teachers of invasive bedside procedures may have inborn traits, I believe behaviors that demonstrate effective teaching can be taught and, with effort, can be mastered. Our results highlight the importance of the teacher’s behaviors with the 3 most common behaviors being pre-briefs, giving performance feedback, and providing autonomy. This was seen in both the fellow and faculty focus groups.
Educators and program leaders could utilize this information in the formation of faculty development geared at improving procedural teaching. From this study, teachers could work to incorporate behaviors known to be effective into their own practice, such as pre-briefs, being clear with feedback and avoiding vague terms, and debriefing after the procedure. We are working on the creation of an assessment tool that we hope to have out in the next year to help with the process of faculty development. The main takeaway is that we, as teachers, can and should get better at teaching ICU procedures!
Blog post author

Dr. Adelman is an Assistant Professor of Medicine at NYU Grossman School of Medicine, and serves as the Medical Director of the Intermediate-Intensive Care Unit at NYU Langone Hospital-Brooklyn, where he is also a site director and an assistant program director for the NYU pulmonary and critical care medicine fellowship program. His research interests include procedure competency assessment methods among GME training programs, in particular point-of-care ultrasound, and high-fidelity medical simulation activities that incorporate virtual reality headsets.
Article author

Dr. Diana Kelm is a core faculty physican in the Division of Pulmonary and Critical Care Medicine at Mayo Clinic Rochester and Assistant Professor of the Mayo Clinic College of Medicine. She is the associate program director for the Pulmonary and Critical Care Medicine fellowship program and is the IM residency MICU rotation director. She is a clinician educator and education science researcher with a research focus on procedural training and interprofessional education.