Beyond the ICU Rotation: The Importance of Trainee Involvement in Post–Intensive Care Unit Clinics
Citation: Ohnigian, S. E., Hall, M. M., Hayes, M. M., & Maley, J. H. (2022). Beyond the ICU Rotation: The Importance of Trainee Involvement in Post–Intensive Care Unit Clinics. ATS scholar, 3(2), 180-187.
Summary
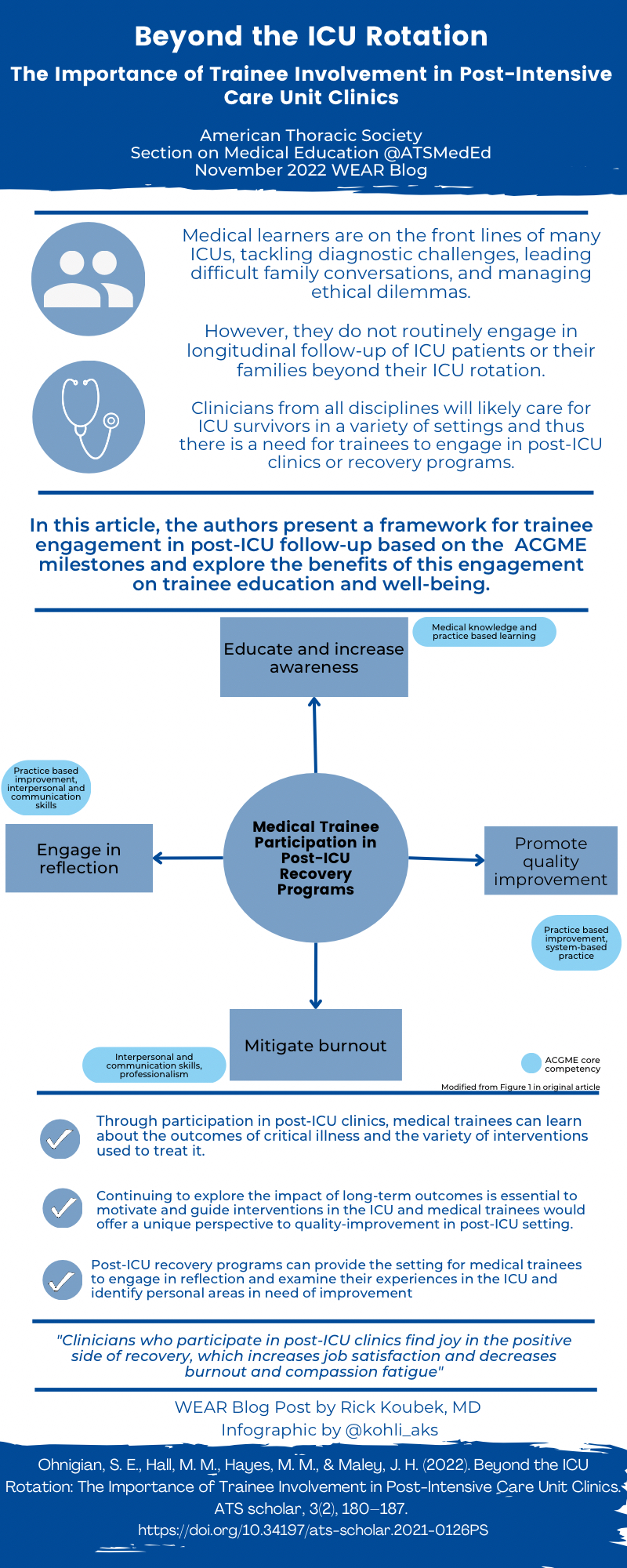
Throughout undergraduate and graduate medical education, many trainees engage in learning through critical care-based rotations in intensive care units (ICUs). An increasingly recognized aspect to the care of critical care patients is after the acute setting through post-ICU clinics and recovery programs, however many learners are not included in this valuable experience. The authors set out to explore the effect of these programs on trainee education by proposing a framework based on the Accreditation Council for Graduate Medical Education milestones. They also describe potential benefits in regard to post-ICU care, family support, ICU quality improvement, as well as allowing for reflection and mitigation of compassion fatigue and burnout.
Interview
RK: As the value of post-ICU clinics in clinical care is increasingly recognized, your article raises a fascinating perspective on their potential value in medical education, as well. What in your own experiences with medical education inspired you to write this article?
SO: During my training, I loved working in the fast-paced ICU and collaborating with a dedicated team of providers all set with a common goal of providing the best life-altering care to our patients. At times the 28-hour shifts were packed with those overwhelming life-altering decisions. As a trainee, I did not always feel closure with those decisions as the patient moved on to the medical floor to continue treatment or they died and their family left the hospital to grieve.
One week, we had a lecture given by Dr Jason Maley, one of my co-authors on this paper, on Post-Intensive Care Syndrome (PICS) and post-ICU clinics, and I was shocked by the innumerable effects that critical care has on our patients and their families for years after. I started evaluating my clinical decisions in a different lens, thinking about not only the immediate ramifications but the possible consequences down the line. As an institution, we have always had an emphasis on quality improvement, but as a trainee, I then felt more of a buy-in to make these changes as I recognized the positive impact they had on patients.
Lastly, I feel that the multidisciplinary approach to post-ICU clinics allows the power of shared reflection to be achieved. As a trainee, there were times when someone read a patient's letter to the ICU sent months after their illness. In that moment, we all felt a strong sense of community and togetherness that seemed scarce, especially during the peak of the COVID-19 pandemic. I truly believe that trainees have a place in post-ICU clinical care for these benefits of engaging in quality improvement, sharing in reflection, and re-discovering and validating the work that they do every day.
RK In what ways do you feel the COVID-19 pandemic has influenced the potential benefits of incorporating residents into post-ICU clinics?
SO: The COVID-19 pandemic hit during the middle of my intern year. I think that it affected each person differently, but I can say that personally, I was extremely distressed by the aforementioned life-altering decisions that we had to make. These decisions felt even more unsettling as we had no idea what would work nor what the long-term outcomes would be. Many times, we were also engaging in care that felt depersonalized, with patients hooked up to ventilators and lines, with their patients on the telephone and not at the bedside. This was a very isolating place for us all to be.
I believe that post-ICU clinics could help manage many of those feelings that I and many of us have had. Post-ICU clinics are a way to engage impressionable trainees in discussion, reflection, and validation regarding these clinical encounters we all face. They create a safe environment with a shared goal of evaluating the care we provide and creating sustainable change for our future clinical care. In that way, those overwhelming life-altering decisions can feel less intimidating and isolating, but rather feel more supported and outcome-driven.
RK What practical tips do you have for program directors and faculty interested in introducing a post-ICU clinic experience into resident medical education?
SO: In this article, we focus on the possible benefits that post-ICU clinic experience could have for trainees. More research and experience in implementation of such a program is necessary for us to be able to make recommendations on curricular change.
RK What do you feel would be the impact to patients of incorporating residents into post-ICU clinics?
SO: Residents are important stakeholders in patient care. For many patients, residents are the first physicians at bedside to evaluate them. For many families, residents are the first physicians to contact them and help guide them through the process. Therefore, it would be beneficial to welcome the perspective and experience of resident physicians into post-ICU clinics for us to improve and also validate their care practices, all with the intent to improve future patient and family outcomes.
RK For those practicing at institutions currently without post-ICU clinics, are there alternative ways they incorporate the principles of your framework into the resident education experience to achieve some of the benefits you propose in your article?
SO: A great start is building awareness of PICS and PICS-F by introducing these topics into general educational conference time. Programs could invite ICU survivors and family members to present their experience at house staff conferences. In addition, simply allowing space during the ICU rotation for reflection would be quite valuable as well.
Blog Post Author

Rick Koubek, MD is a Pulmonary and Critical Care Medicine physician and Clinical Assistant Professor of Medicine at Spectrum Health/Michigan State University in Grand Rapids, MI. He has specific interest in curriculum design, simulation-based learning, and procedural teaching.
Article Author

Sarah Ohnigian, MD is an academic hospitalist at Beth Israel Deaconess Medical Center and Instructor of Medicine at Harvard Medical School. She is passionate about leading teams with the goal of providing excellent clinical care to patients and educating peers and trainees to do the same all while building and maintaining the intellectual curiosity that drives us all.
Twitter: @SarahOhnigian
Trainee Takeaway
This article was very interesting to me as a trainee interested in critical care medicine and as a family member of someone impacted by post-intensive care syndrome. The article is unique in that it addresses the benefits of a post-ICU curriculum on both patient care and trainee well-being. As a future medical educator, the emphasis on developing a curriculum based on ACGME core competencies ensures that training programs can effectively implement strategies without disrupting existing educational models. I am looking forward to participating in post-ICU care clinics and eventually playing a greater role in promoting PICS prevention and awareness.

Sriram Sunil Kumar, MBBS is an aspiring clinician-educator and an applicant for internal medicine residency this match cycle. He graduated from Bangalore Medical College and Research Institute in Bangalore,India. and has interests in critical care medicine, high-value healthcare, and global health.
Twitter: @sriramsunilk