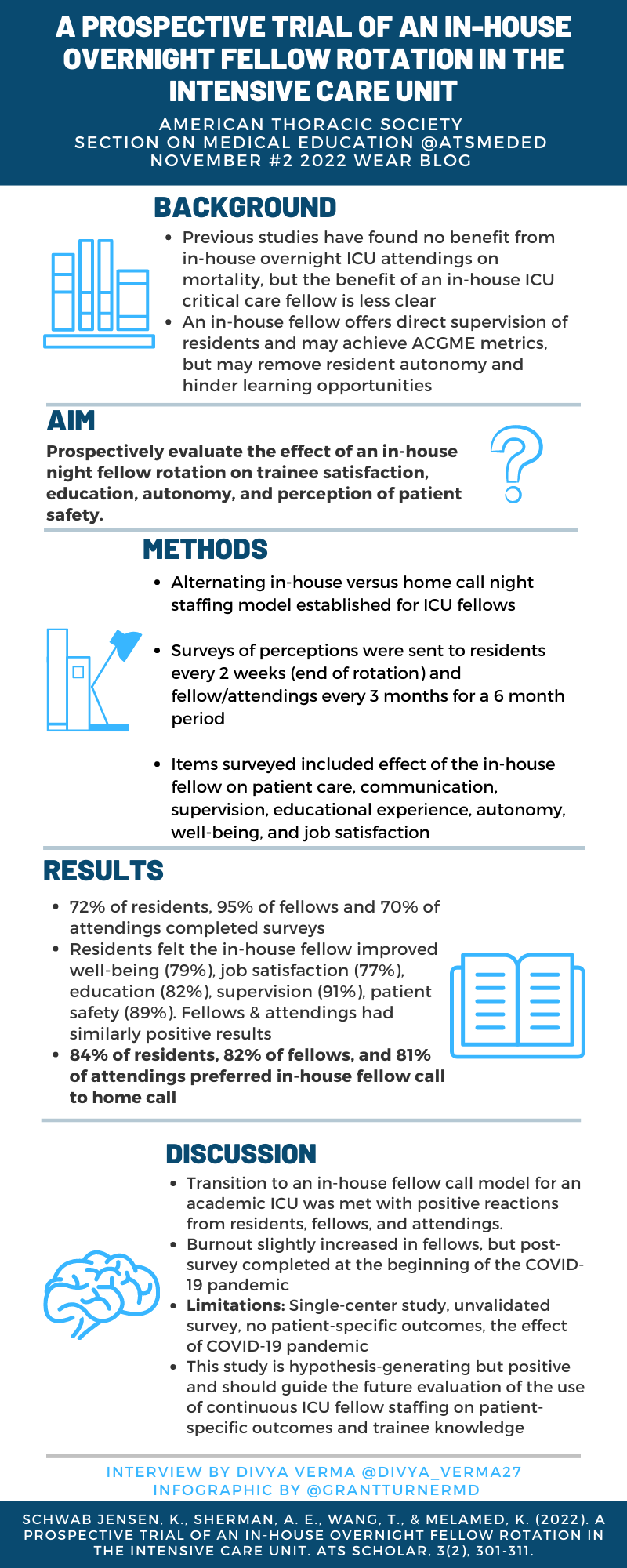
A Prospective Trial of an In-house Overnight Fellow Rotation in the Intensive Care Unit
Schwab Jensen, K., Sherman, A. E., Wang, T., & Melamed, K. (2022). A Prospective Trial of an In-house Overnight Fellow Rotation in the Intensive Care Unit. ATS Scholar, 3(2), 301-311.
Summary
This study set out to define the impact of overnight in-house ICU coverage by fellow physicians on trainee education and well-being. The authors conducted a prospective trial alternating two weeks of in-house ICU fellow coverage with two weeks of home call coverage in a tertiary medical center ICU over a period of six months. They then surveyed residents, fellows, and attendings to evaluate perceptions of the night fellows' impact on patient care, educational experience, autonomy and well-being amongst other variables. They found that a majority of those surveyed felt that having an in-house fellow led to perceived improvement in patient care as well as significant improvement in resident education, along with a simultaneous positive impact on fellow well-being.
Interview
DV: How did you select the outcomes that were studied in this article?
KSJ: We used prior research that examined the impact of in-house attendings to help guide us. These studies, which looked at patient outcomes such as mortality, did not show a benefit to in-house attending staffing - and so we decided to broaden the question beyond just patient outcomes. We focused on outcomes centered on the trainee experience: housestaff wellbeing and housestaff education. While we also examined perception of patient care, we didn't want this to be the sole focus of the paper.
DV: How have the results of this study impacted your institution's practices re: in-house fellow coverage? Is this different across different clinical sites?
AS: We have continued in-house fellow coverage. While it transitioned from a research study into standard practice because of the COVID-19 pandemic, it has remained an integral part of our institution's fellow coverage.
DV: Given the positive impact that adding a fellow had on resident perceptions of education and wellness, would you expect a similar effect on fellow perceptions of education and wellness with the addition of an in-house attending?
AS: Being the in-house fellow without an in-house attending presents a unique level of responsibility and independence not always present in a quaternary care hospital. The night fellow fills the role of an in-house attending for the residents overnight. One of our attendings even commented that they thought the presence of a fellow was perhaps superior to having an attending physician!
KSJ: Yes! Along those lines, I think that there are many ways in which a fellow might actually represent the perfect middle ground for overnight supervision. They offer an added layer of experience, but are presumably more approachable and less intimidating than an in-house attending. It would have been interesting if we had asked residents in the survey whether they would have preferred in-house attendings or in-house fellows!
DV: What did you think was the most striking or unexpected result of this study?
AS: I was most surprised by the nearly unanimous positive response to the addition of an in-house night fellow. Even amongst the fellows that were now having to stay overnight, people responded favorably and felt this had a positive impact.
KSJ: I was surprised that residents did not really feel like an in-house fellow negatively impacted their degree of autonomy overnight. When designing the in-house rotation, we tried to ensure that residents still took the "first pass" with all patient-care related issues - only reaching out to the fellow once they had formulated their own assessment and plan. The fact that this worked - and that residents still felt autonomous and independent - is encouraging to me.
DV: Has there been a change in patient outcomes since the implementation of an in-house fellow?
AS: We would have loved measure this, but there are countless confounders impacting patient outcomes, and we felt it could be misleading regardless of the findings. Anecdotally, I do believe there has been improved progression of care in the ICU patients overnight.
KSJ: Yes, I think this could be a future study - comparing whether certain quality of care metrics (such as length of ICU stay, or bundle compliance, or patient satisfaction) changed after implementation of this in-house fellow rotation. Hopefully this study is just the first of many - so stay tuned!
Blog Post Author

Divya Verma is a first year pulmonary and critical care fellow at Emory University. She loves medical education and working with learners at all levels and is excited to find her niche within PCCM over the next few years.
Twitter: @divya_verma27
Article Authors

Kristin Schwab Jensen is an assistant clinical professor in the division of Pulmonary and Critical Care at UCLA, where she co-directs the Post-ICU Recovery Clinic and directs the Pulmonary Rehabilitation program. She is very invested in medical education. She is an associate program director for the UCLA Internal Medicine Residency program. She is also involved with the ATS Critical Care Committee.
Twitter: @CritKristin
Alex Sherman is a Clinical Instructor in Pulmonary & Critical Care Medicine at UCLA where he cares for patients with pulmonary hypertension and pulmonary vascular disease. He directs the invasive cardiopulmonary exercise lab and is heavily invested in medical education.
Twitter: @alexshermanMD