Article:
“A National Survey of Burnout and Depression Among Fellows Training in Pulmonary and Critical Care Medicine: A Special Report by the APCCMPD”.
Responses from first Author: Michelle Sharp, MD, MHS
Additional Responses from Gabe Bosslet MD, APCCMPD President and Kristin Burkart MD MSc, Chair of the ATS Training Committee
Summary:
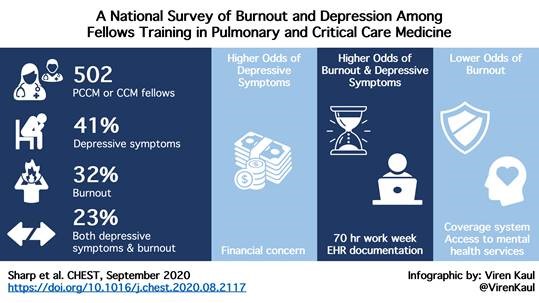
Sharp and colleagues set out to investigate the burden of burnout and mental health disturbances in pulmonary and critical care fellows in a national survey. Nearly one-thousand fellows responded and over half screened positive for burnout or depression in a cross-sectional electronic survey of fellows enrolled in pulmonary, PCCM, and critical care training programs. Symptoms of depression and burnout were assessed via the Maslach Burnout Index two-item questionnaire and the Primary Care Evaluation of Mental Disorders. Almost 40% of respondents reported over $200,000 in student loan debt. The researchers note over 40% of respondents met criteria for clinical depressive symptoms, 32% had symptoms of burnout, and nearly a quarter (23%) had symptoms of both depression and burnout. Higher odds of burnout were noted in fellows reporting more than 70 hours on average of clinical work. Higher odds of depressive symptoms were noted in those with concurrent financial concerns and those working more than 70 hours in a work week. The burden of electronic health records was also noted by both respondents reporting depressive and burnout symptoms. Of those reporting a back-up coverage system, nearly 1/3 felt uncomfortable accessing this system. Likewise, among respondents reporting access to mental health resources, 15% said they were reluctant to utilize these resources. Utilization of these resources by training programs was not evaluated. Given the high prevalence of depressive symptoms and burnout in trainees of PCCM, systemic solutions at a programmatic and systemic level are needed. In addition, this research was prior to the COVID-19 pandemic, and given these respondents are now working in the pandemic, there is an urgent need to address this public health crisis in the Graduate Medical Education community.
Interview:
NHS: How did you decide to look into this issue?
MS: I experienced burnout during my Assistant Chief of Service (ACS) year (a Medicine Chief year with full time clinical service and mentoring residents - worked ~80-100 hours for most of the year). I saw a lot of burnout among friends and residents I was mentoring. I read a lot about it following my Chief year and wrote a review which gave me the opportunity to learn what other fields (business world) do to address burnout. I wanted to understand/learn about the level of burnout and depression in PCCM and possible drivers of burnout and depression beyond individual factors (programmatic and institutional).
NHS: What are 1-2 important things you learned during this project?
MS: A coverage or jeopardy system was something I was very interested in looking into in terms of burnout. As I had experienced having to choose between family events (weddings/funerals/illness) and my clinical duties during my training. It can be quite stressful to arrange coverage to make it to the important events especially in urgent situations. There is also a culture at some institutions that calling out even for illness is a sign of weakness.
Our results showed that the presence of coverage systems and mental health resources were associated with lower odds of burnout, but that fellows were not always aware of the systems in place. This surprised me. The importance of communicating policies and presence of mental health resources and coverage systems to trainees was something that I learned from this project.
NHS: What is the most important “take away” or piece of advice for trainees dealing with burnout?
MS: My biggest take away was that burnout and/or depression affected 1/2 of the respondents. More research needs to be done to investigate the possible drivers and interventions to see if they will lead to improvement. Something we can all do in the meantime is check in with trainees and each other and encourage self-care.
Interview with Dr. Gabe Bosslet, APCCMPD President and Kristin Burkart
NHS: What is one piece of advice for faculty educators or program directors to help mitigate burnout for their trainees?
GB: Program Directors should pay attention to the process of being a fellow and attend to this process. Ask about mental health and how fellows are doing- do this in a personal way and in a forum that allows for openness and vulnerability. Be prepared to provide “wellness days” for those rotations that approach 70 hours of worktime per week and make the system for taking these days simple and non-punitive for trainees. Lastly, Program Directors should model the behavior they want to see in their trainees. Give personal examples of when you have had to ask for help and give kudos to those who have been champions of wellness within the training program.
KB: It is known that systems and processes are significant drivers of burnout and strategies implemented at the organizational level have been shown to be effective in decreasing physician burnout. We can and should pay attention to the schedule and work to balance high-intensity rotations (ones that are typically >70 hours per week) with lower-intensity rotations (ones that are typically <70 hours per week) and aim to have fellows work no more than 12 weekends a year. Program Directors need to empower, support, and normalize fellows’ use of coverage systems and institutional mental health resources. As leaders, we must also role model behaviors and values we wish to instill within our fellows and talk openly about our struggles and strategies we use to enhance our wellbeing and fight burnout.
Conclusions:
Given the pervasive nature of burnout and depression not only in medicine in general, but specifically in pulmonary and critical care trainees, it is vital we be aware of this and evermore active in checking on our colleagues. It is also imperative that training programs make trainees aware of programmatic and systemic opportunities to seek assistance if necessary, and to encourage an open dialogue on these issues with their trainees.
Blog Post Author

Dr. Nancy H Stewart is an Assistant Professor of Medicine in the Division of Pulmonary, Critical Care, and Sleep Medicine at the University of Kansas. She earned a B.A. in Biochemistry and a B.A. in German both from the University of Mississippi, and her D.O. from Kansas City University of Medicine and Biosciences. She completed residency in Chicago followed by a Medical Education fellowship and a Hospital Research Fellowship at The University of Chicago. She completed Pulmonary, Critical Care, and Sleep Medicine fellowships in Omaha, Nebraska prior to joining faculty at The University of Kansas. Her research focuses on improving care and outcomes for patients with COPD/OSA Overlap Syndrome. She also is interested in improving medical education for trainees across the training spectrum.
Twitter: @nvhstewart
Article Authors

Dr. Michelle Sharp is an Assistant Professor in the division of Pulmonary and Critical Care Medicine at the Johns Hopkins University School of Medicine and she serves as the Co-Director of the Johns Hopkins Sarcoidosis Program. Dr. Sharp earned a B.S. from Tulane University and her M.D. from Louisiana State University School of Medicine. She completed residency and fellowship training at Johns Hopkins University School of Medicine and was an Assistant Chief of Service of the Osler Medical Service. Dr. Sharp’s research is focused on improving clinical outcomes for patients with sarcoidosis. She additionally has interests in physician burnout and patient centered care.
Twitter: @mwsharp5

Dr. Kristin M Burkart is a Pulmonary and Critical Care Physician and an Associate Professor of Medicine at Columbia University Medical Center. She is the Director of the Pulmonary and Critical Care Fellowship Training Program and the Medical Director of the Chest Clinic. Dr. Burkart graduated AOA from Albany Medical College, completed her residency and chief residency at the University of Colorado and completed her fellowship in Pulmonary and Critical Care Medicine at Boston University School of Medicine. She has a Master of Science in Epidemiology from Boston University School of Public Health. She is a Past President and currently serves on the Board of Directors of the Association of Pulmonary and Critical Care Medicine Program Directors(APCCMPD). Dr. Burkart is the Chair of the American Thoracic Society (ATS) Training Committee, Chair of the APCCMPD Education Committee and a Deputy Editor for ATS Scholar. Her academic interests include faculty development, GME program leadership and advocacy and physician wellbeing.
Twitter: @KristinBurkart3

Dr. Gabriel Bosslet is currently the President of the Association of Pulmonary and Critical Care Medicine Program Directors. He is an Associate Professor for Clinical Medicine at Indiana University, where he is also the Pulmonary and Critical Care Medicine Fellowship Director and an Assistant Dean for Faculty Affairs and Professional Development.
Twitter: @gbosslet
Article Citation: Sharp M, Burkart KM, Adelman MH, Ashton RW, Biddison LD, Bosslet GT, Doyle ST, Eckmann T, Khurram S Khan MM, Lenz PH, McCallister JW, O'Toole J, Rand CS, Riekert KA, Soffler MI, Winter GR, Zaeh S, Eakin MN. "A National Survey of Burnout and Depression Among Fellows Training in Pulmonary and Critical Care Medicine: A Special Report by the APCCMPD. Chest. 2020 Sep 18:S0012-3692(20)34511-6. doi: 10.1016/j.chest.2020.08.2117. Epub ahead of print. PMID: 32956717.



