Telerehabilitation has the potential to overcome known barriers to pulmonary rehabilitation participation and could be a relevant treatment alternative across all chronic respiratory diseases. However, and rightfully, many healthcare professionals are still skeptical in terms of the effectiveness, safety and its ability to deliver “proper” pulmonary rehabilitation.
The COVID-19 pandemic has pushed to an unforeseen “emergency” transition of conventional pulmonary rehabilitation programs to a delivery format of telerehabilitation of various contents and formats in clinical practice. The transition stresses the importance of a collective update on telerehabilitation. We are therefore looking forward to the Cochrane review on telerehabilitation for chronic lung diseases, from Professor Hollands group, which would be a timely published and comprehensive update during the challenging COVID-19 pandemic1.
Our research group recently published a proposal on a supervised pulmonary telerehabilitation (PTR) program which may be suitable as a second-choice alternative to conventional PR2. Indeed, we feel confident that the upcoming Cochrane review will support that PTR is effective, safe and a highly relevant second choice alternative to conventional PR.
Still, reading the existing literature on PTR many questions remain unanswered. We are aware of nine published RCT delivering primary PR while using different information and communication technology (ICT) (figure 1)2–10. Besides obvious differences in ICT, content and duration, a brief scan of the RCT studies reveals that the level of the participants technical skills is sparsely stated. One could assume that a vast majority of the selected participant have a positive attitude towards ICT solutions and their own technical capabilities. If so, is this the general attitude and capability in the group of many, that we want to target and offer these alternative solutions for?
Essentially, future telerehabilitation designs must include specific considerations regarding delivery form and content and definition of technical skills of the targeted population, particularly if PTR is to be considered as an extended offer specifically to those who live remotely and to those who lack energy and resources to join a conventional out-patient PR program.
Future research must continue to address which patients are best suited to telerehabilitation and how we accommodate the increasing focus on personalized training. We need further understanding on how to ensure sufficient digital literacy and subsequently ways to promote it among our elderly and frail patients.
We are not aware of any studies comparing non- or partly supervised ICT delivered PR with fully supervised PTR. It is out impression that the existing evidence on PTR is at a reasonable level where “internal” ICT comparisons on effectiveness and costs is requested; e.g. supervised video-based PTR with individual home-based telephone call supported PR. Subsequently, the comparisons must include long-term effects and behavioral sustainability which is less convincing in the existing literature3,7,11.
Lastly, it would be interesting to read RCTs that specifically attempted to recruit patients unwilling to participate in conventional out-patient PR with real-world inclusion/exclusion criteria. A detailed consort diagram of eligible and included would be of similar interest and relevance as the actual results from such study.
The various ways of delivering telerehabilitation, has been nicely outlined by Dr. Narelle Cox and Professor Anne Holland in a previous Quarterly bite, and we warmly recommend you read it.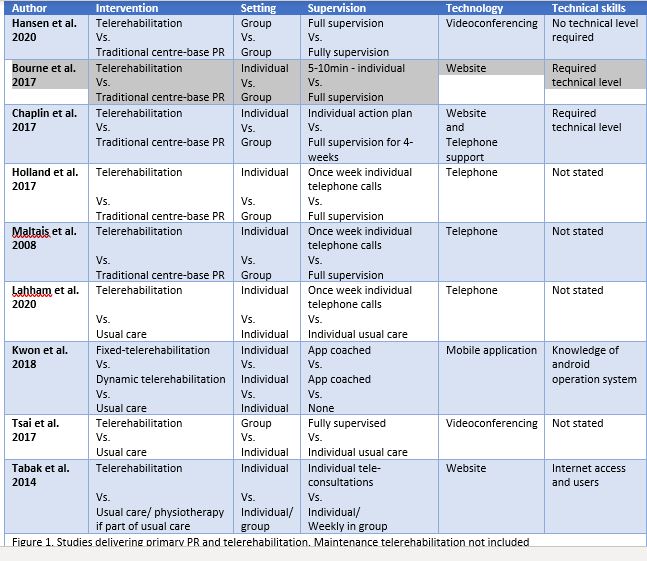 References
References
- Cox NS, MaDonald CF, Hill JC, et al. Telerehabilitation for chronic respiratory disease (protocol). Cochrane Database Syst Rev. 2018;(6). doi:10.1002/14651858.CD013040
- Hansen H, Bieler T, Beyer N, et al. Supervised pulmonary tele-rehabilitation versus pulmonary rehabilitation in severe COPD: a randomised multicentre trial. Thorax. March 2020:thoraxjnl-2019-214246. doi:10.1136/thoraxjnl-2019-214246
- Holland AE, Mahal A, Hill CJ, et al. Home-based rehabilitation for COPD using minimal resources: A randomised, controlled equivalence trial. Thorax. 2017;72(1):57-65. doi:10.1136/thoraxjnl-2016-208514
- Bourne S, DeVos R, North M, et al. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomised controlled trial. BMJ Open. 2017;7(7):e014580. doi:10.1136/bmjopen-2016-014580
- Chaplin E, Hewitt S, Apps L, et al. Interactive web-based pulmonary rehabilitation programme: a randomised controlled feasibility trial. BMJ Open. 2017;7(3):e013682. doi:10.1136/bmjopen-2016-013682
- Tsai LLY, McNamara RJ, Moddel C, Alison JA, McKenzie DK, McKeough ZJ. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: The randomized controlled TeleR Study. Respirology. 2017;22(4):699-707. doi:10.1111/resp.12966
- Maltais F, Bourbeau J, Shapiro S, et al. Annals of Internal Medicine Article Effects of Home-Based Pulmonary Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease. Ann Intern Med. 2008.
- Kwon H, Lee S, Jung EJ, et al. An mHealth management platform for patients with chronic obstructive pulmonary disease (Efil breath): Randomized controlled trial. JMIR mHealth uHealth. 2018;6(8). doi:10.2196/10502
- Lahham A, McDonald CF, Moore R, et al. The impact of home‐based pulmonary rehabilitation on people with mild chronic obstructive pulmonary disease: A randomised controlled trial. Clin Respir J. 2020;14(4):335-344. doi:10.1111/crj.13138
- Tabak M, Brusse-Keizer M, van der Valk P, Hermens H, Vollenbroek-Hutten M. A telehealth program for self-management of COPD exacerbations and promotion of an active lifestyle: A pilot randomized controlled trial. Int J COPD. 2014;9:935-944. doi:10.2147/COPD.S60179
- Godtfredsen, NS, Hansen H et al. 12-months follow-up of pulmonary tele-rehabilitation versus standard pulmonary rehabilitation: A multicentre randomised clinical trial in patients with severe COPD. Respir Med. 2020;Accepted for publication.



