Contributed by Isabelle Boutin, MD, Isabelle Coté, MD, and R. John Kimoff, MD, Respiratory Division & Sleep Laboratory, McGill University Health Centre, Montreal, Quebec Canada
A 56 y old female diagnosed with severe OSA (AHI 67 events/h) two years ago had had an excellent symptomatic response to nasal CPAP at 10 cm H2O. Excessive daytime sleepiness had resolved and her productivity at work had increased substantially. However over the past 4-5 months she notes that she wakens several mornings per week feeling much less refreshed, and on some of these days she again experiences sleepiness which affects her work.
Her weight is unchanged; she does not use alcohol and she is taking no new medications. She has no ENT complaints other than mild intermittent nasal stuffiness on CPAP, and does not report oral dryness during the night or in the morning. She uses the same nasal CPAP mask and headgear every night and uses heated humidification. Her CPAP unit has been verified by the supplier to be delivering 10 cm H2O. This setting was based on a satisfactory manual polysomnographic titration study at the time of treatment initiation.
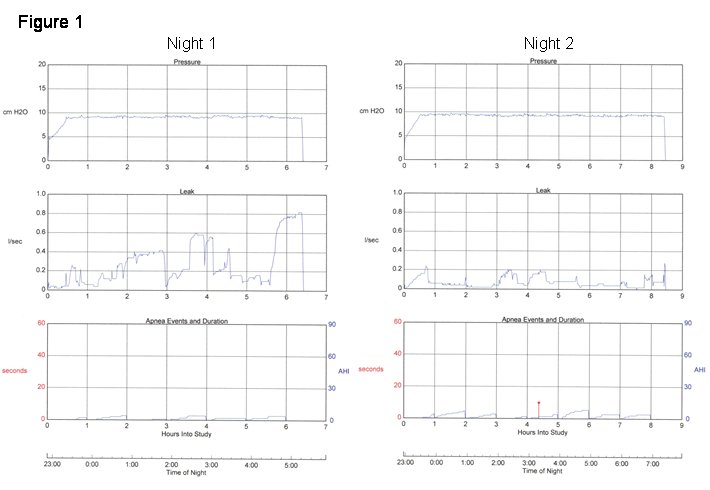
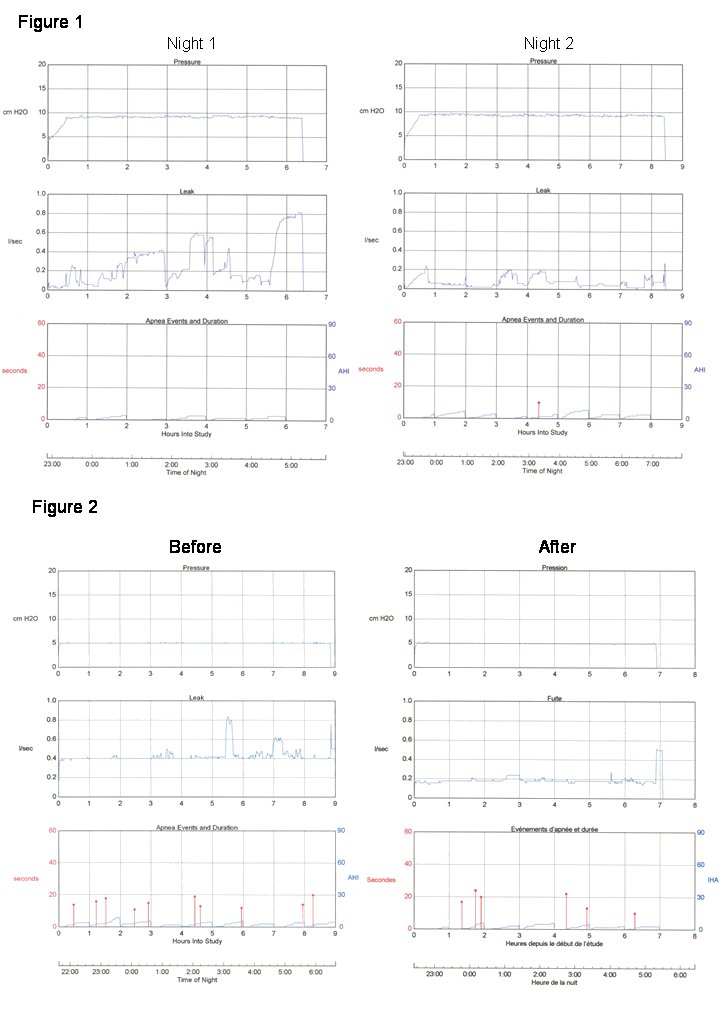
Current adherence data from her CPAP unit show only rare missed nights and fairly consistent nightly use times with a mean of 7 h, 32 min. per night. The reported residual AHI value is 4.3 events per hour, with little variability from night to night. However, nightly values for the 95th percentile leak vary considerably around the manufacturer's recommended maximum of 0.4 l/s, with values ranging from 0.2 to as high as 0.8 l/s. Two representative nights are shown in Figure 1.
Question #1: What might account for the difference in leak between these 2 nights?
Case #2
A 62 year old woman diagnosed with moderate OSA (AHI 38 events/h) was treated with nasal CPAP 5 cm H2O based on a manual titration polysomnogram with good symptomatic response. After several years on treatment, the patient began to feel that her sleep was not as refreshing. She returned for clinical re-evaluation, bringing adherence data from her CPAP machine.
When she was informed that the reported leak levels on the download were significantly higher than previously observed, she immediately indicated that she knew what the problem was and how to fix it. She sent in new adherence data one month later and reported feeling "almost back to normal".
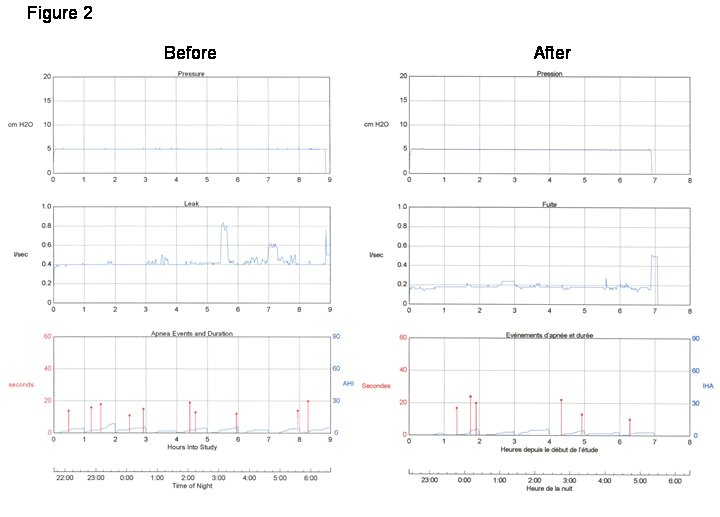
Figure 2 shows adherence data from 2 representative nights prior to and following the patient’s "intervention" with her equipment.
Question #2: What does the pattern of leak suggest about its cause and what might the patient have done to rectify the leak?
Discussion Case #1
The left panel of Figure 1 shows several periods of high leak. The leak could be partly explained by the presence of mouth leak, but the absence of oral dryness with significant leak makes this much less likely. Another explanation could be mask displacement following changes in head or body position. The right hand panel shows a similar pattern of leak variability but at much lower levels.
Upon close questioning, the patient indicated that several nights per week, she was using hair curlers. On those nights she would loosen her CPAP headgear considerably to accommodate the curlers. She had been doing this since changing hair styles approximately 5 months earlier, which coincided with the intermittent return of daytime symptoms.
When asked to document the relationship between curler use, nightly leak values and daytime symptoms using a sleep diary, she subsequently confirmed that there was indeed a close relationship. While the patient was reticent to change her hairstyle, changes in curler size and headgear adjustment have led to a considerable improvement.
It is noteworthy that on high leak nights, the reported residual AHI values were not higher than on the low leak nights, despite a difference in symptoms. This could reflect either the reduced accuracy of software event detection with high leak, or increased sleep fragmentation independent of respiratory events which can occur with leak, or both.
Discussion Case #2
The most striking aspect of the leak pattern in both panels of Figure 2 is the constant elevated baseline value across the entire night. Leak on the "before" night is high (at the manufacturer’s threshold "acceptable" value), and on the "after" night is considerably lower but still present. The constant baseline leak is suggestive of an improperly fitted connection or open pressure port on a mask.
The patient reported having several cats who were very attracted to the CPAP equipment, and chewed on the tubing, resulting in multiple holes in the tubing. The patient’s solution was to repair the tubing with duct tape, which improved, but did not completely resolve the leak as some of the holes were very small and missed.
She subsequently replaced the tubing, only to have the problem recur, until more recently, she acquired a sleeve for her tubing designed to augment humidity. This has proven to be a very effective deterrent to the cats.
General Discussion
Excessive leak during CPAP may compromise treatment efficacy by increasing respiratory events (1), increasing sleep fragmentation (2) and reducing compliance (3,4). Leak particularly compromises the responses of auto-adjusting CPAP (1,5), and it also reduces the reliability of the reported respiratory event indices from CPAP adherence monitors.
Excessive leak is now often identified from CPAP adherence monitors. Total CPAP leak is the sum of intentional mask leak to prevent CO2 rebreathing and unintentional leak. Some manufacturers report total leak, while others report only unintentional leak. It is therefore essential to be aware of which is being reported, and what the recommended threshold values are, for proper interpretation of device data. As illustrated by these two cases, the pattern of leak from the CPAP adherence monitors may provide clues as to its cause, although clinical data are also essential.
The most common sources of leak are mouth opening during nasal mask use, and leak due to suboptimal headgear adjustment and mask displacement, as in Case 1. Excessively worn or broken masks and headgear favor leak, and tubing or connector problems may be a factor as illustrated in Case 2. Aerophagia can contribute to leak as the swallowed air is not expired and most leak algorithms involve detection of inspiratory vs expiratory flow discrepancies (2). Rare causes of leak include intra-cranial leak producing pneumocephalus in patients with previous sinus or skull surgery or trauma (6), and retrograde lacrimal duct leak with eye irritation (7).
Oral dryness strongly suggests mouth leak, although the absence of dryness does not preclude significant mouth leak (2,3). Nasal congestion may both result from, and in turn worsen mouth leak (3,8). Bed partner observation of mouth opening or mask displacement may be helpful if present. Direct inspection of the patient’s equipment and how it is applied can be very instructive. This can be done in an outpatient context or during laboratory polysomnography.
At polysomnography, leak is manifested by transient or persistent reduction of CPAP below the set level, and/or by a positive baseline offset of CPAP or pneumotachographic flow signals. The source of leak can be identified by video or direct bedside observation of mask placement and/or mouth opening, and by the use of an oral thermistor or capnography to detect leak at the mouth or around the mask.
Management of leak includes optimization of mask and headgear fit, comfort and seal and comfort, verifying the integrity of the circuit, and use of heated humidification, with in some instances nasal lubricant or inhaled steroid, to minimize nasal symptoms (4,8,9). Mouth leak can be improved by use of a chin strap, placement of tape or a bandage over the mouth, or use of a full face or oral interface (9). Fixed CPAP should be prescribed at the lowest effective level to minimize leak. In some cases, the addition of expiratory pressure reduction or use of auto-adjusting CPAP which lowers mean pressure may improve leak.
References
- Collier D, Stanley D, Parthasarathy S. Effect of air leak on the performance of auto-PAP devices: a bench study. Sleep Breath 2005; 9:167-75.
- Teschler H, Stampa J, Ragette R, Konietzko N, Berthon-Jones M. Effect of mouth leak on effectiveness of nasal bilevel ventilatory assistance and sleep architecture. Eur Respir J 1999;14:1251-7.
- Baltzan MA, Elkholi O, Wolkove N. Evidence of interrelated side effects with reduced compliance in patients treated with nasal continuous positive airway pressure. Sleep Med 2008, doi:1016/j.sleep.2007.12.005.
- Massie CA, Hart RW, Peralez K, Richards GN Effects of humidification on nasal symptoms and compliance in sleep apnea patients using continuous positive airway pressure. Chest 1999; 116: 403-8.
- Farré R, Montserrat JM, Rigau J, Trepat X, Pinto P, Navajas D. Response of automatic continuous positive airway pressure devices to different sleep breathing patterns: a bench study. Am J Respir Crit Care Med 2002; 166:469-73
- Jarjour NN, Wilson P. Pneumocephalus associated with nasal continuous positive airway pressure in a patient with sleep apnea syndrome. Chest 1989; 96:1425-6.
- Waller EA, Bendel RE, Kaplan J. Sleep disorders and the eye. Mayo Clin Proc 2008; 83:1251-61.
- Richards GN, Cistulli PA, Ungar RG, Berthon-Jones M, Sullivan CE. Mouth leak with nasal continuous positive airway pressure increases nasal airway resistance. Am J Respir Crit Care Med 1996;154:182-6.
- Martins De Araújo MT, Vieira SB, Vasquez EC, Fleury B Heated humidification or face mask to prevent upper airway dryness during continuous positive airway pressure therapy. Chest 2000 ;117:142-7.