Contributed by Sushmita Pamidi, M.D., Instructor of Medicine, Section of Pulmonary and Critical Care Medicine, University of Chicago, Babak Mokhlesi, M.D., M.Sc., Associate Professor of Medicine, Director, Sleep Disorders Center and Sleep Fellowship Program, University of Chicago
A 46 year-old woman on oral and intrathecal narcotics for chronic back pain was referred to our Sleep Disorders Center for a second opinion after intolerance to CPAP for her severe obstructive and central sleep apnea. The patient was taking 10 mg of oral hydrocodone three times daily, in addition to intrathecal dilaudid, bupivicaine, and lidocaine. The patient was unwilling to try other forms of positive airway pressure therapy, including adaptive servoventilation or bi-level PAP with a back-up rate. A repeat split night polysomnogram was performed with the results summarized in the table below.
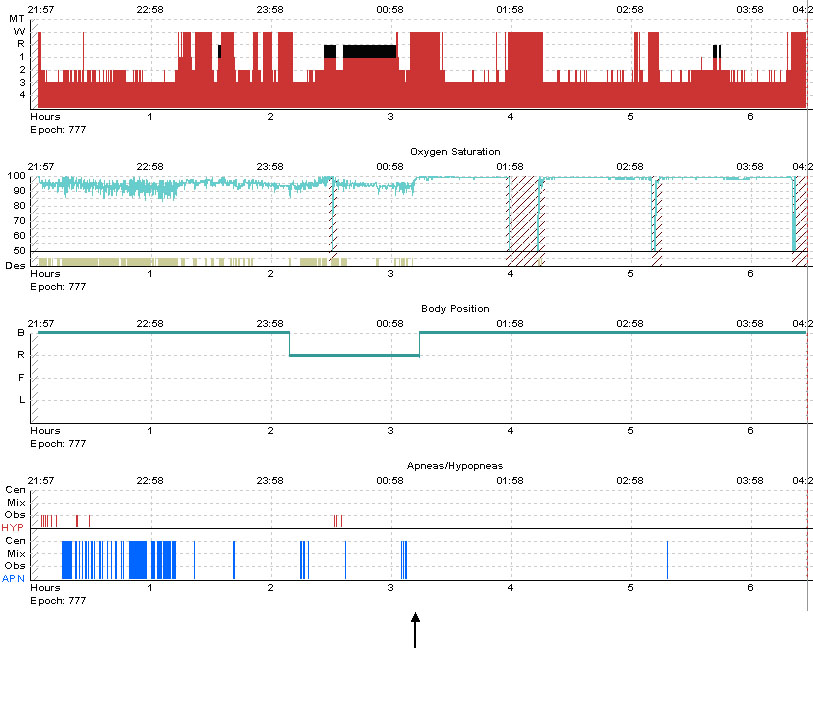
Question: Based on the the hypnogram, what treatment modality was started at the time point indicated by the arrow?
|
|
Pre-Treatment |
On Treatment |
|
AHI (event/h) |
42 |
0.4 |
|
Obstructive AHI (events/h) |
5 |
0 |
|
Central apnea index |
37 |
0.4 |
|
3% oxygen desaturation index (event/h) |
59 |
0 |
|
Arousal Index (event/h) |
18 |
9 |
|
Sleep Efficiency (%) |
78 |
80 |
Answer: Supplemental oxygen was started (2 liters/minute).
As illustrated by the hypnogram, supplemental oxygen at 2 L/min eliminated the central apneas and oxygen desaturations. The patient had very few obstructive events in the pre-treatment part of the study that were comprised of hypopneas associated with desaturations, and not arousals. It is possible that these initial hypopneas were mistakenly labeled as obstructive, rather than central hypopneas. In some cases, it is difficult to make the distinction between central and obstructive hypopneas without the use of esophageal manometry to accurately measure respiratory effort. Upon follow-up after 2 months, she reported a reduction in hypersomnolence, daytime fatigue and an improvement in the quality of her sleep with supplemental nocturnal oxygen therapy.
Central sleep apnea (CSA) may have a variety of etiologies, including high-altitude induced periodic breathing, idiopathic CSA, narcotic-induced CSA,(1, 2) and Cheyne-Stokes breathing. In addition to improving the underlying disease where possible, traditional treatment options involving the application of positive airway pressure (PAP), such as CPAP, bi-level PAP with a back-up rate, and adaptive servoventilation, are commonly used.(3) However, smaller studies have also shown benefit of nocturnal oxygen therapy in some cases of CSA, usually in the setting of heart failure but sometimes due to other causes.(4) In particular, oxygen may be a favorable option in those patients who cannot tolerate PAP therapy.
In the setting of increased ventilatory instability, supplemental nocturnal oxygen has been demonstrated to improve obstructive events, but there is no evidence that the same occurs for central apneas.(5) In addition, Gold and colleagues demonstrated that patients with predominantly central and mixed sleep apnea who received supplemental nocturnal oxygen had a significant reduction in central and mixed respiratory events.(6) However, in these same patients, there was a significant increase in obstructive apneas after oxygen was administered. The mechanism for the increased obstructive apneas is not known, but may be related to changes in the respiratory control system. In this particular patient, however, we did not observe an increase in obstructive events.
It is important to keep in mind that supplemental oxygen administration may decrease the ability to score hypopneas. For example, in this case, there was an absence of oxygen desaturation events after oxygen administration, whereas prior to oxygen administration, the oxygen desaturation index was 59. A decrease in oxygen desaturation events after supplemental oxygen may occur either due to the ability of oxygen to improve central events or due to the improvement in oxygen stores and subsequent amelioration of desaturation events, even if subtle respiratory events persist. In addition, this patient was on several narcotics, and it is possible that these medications increased her arousal threshold, thus also potentially limiting the detection and scoring of obstructive hypopneas. However, this is less likely given that there was a decrease in the arousal index and an improvement in sleep efficiency with supplemental oxygen. Moreover, central apneas were eliminated in this patient with supplemental oxygen and the breathing pattern became more regular.
Long-term studies are needed to further validate oxygen as an effective treatment option in cases such as this. Other treatment options for central sleep apnea include pharmacologic therapies, such as theophylline and acetazolamide, which have been shown to be of some use in sleep-disordered breathing at high altitude.(7) However, most of these studies have not evaluated the role of long-term pharmacotherapy in CSA.(8)
References:
- Farney RJ, Walker JM, Cloward TV, Rhondeau S. Sleep-disordered breathing associated with long-term opioid therapy. Chest. Feb 2003;123(2):632-639.
- Walker JM, Farney RJ, Rhondeau SM, et al. Chronic opioid use is a risk factor for the development of central sleep apnea and ataxic breathing. J Clin Sleep Med. Aug 15 2007;3(5):455-461.
- Javaheri S, Malik A, Smith J, Chung E. Adaptive pressure support servoventilation: a novel treatment for sleep apnea associated with use of opioids. J Clin Sleep Med. Aug 15 2008;4(4):305-310.
- Franklin KA, Eriksson P, Sahlin C, Lundgren R. Reversal of central sleep apnea with oxygen. Chest. Jan 1997;111(1):163-169.
- Wellman A, Malhotra A, Jordan AS, Stevenson KE, Gautam S, White DP. Effect of oxygen in obstructive sleep apnea: role of loop gain. Respir Physiol Neurobiol. Jul 31 2008;162(2):144-151.
- Gold AR, Bleecker ER, Smith PL. A shift from central and mixed sleep apnea to obstructive sleep apnea resulting from low-flow oxygen. Am Rev Respir Dis. Aug 1985;132(2):220-223.
- Fischer R, Lang SM, Leitl M, Thiere M, Steiner U, Huber RM. Theophylline and acetazolamide reduce sleep-disordered breathing at high altitude. Eur Respir J. Jan 2004;23(1):47-52.
- Javaheri S. Acetazolamide improves central sleep apnea in heart failure: a double-blind, prospective study. Am J Respir Crit Care Med. Jan 15 2006;173(2):234-237.