Contributed by Joseph Braidy, MD, of the University of Montreal, Montreal, Canada, and Susheel Patil, MD, of Johns Hopkins School of Medicine, Baltimore, MD
A 38 year old man presented to our Sleep Disorders Clinic with a long-standing history of snoring and witnessed apneas observed by his wife. He also complained of severe daytime somnolence (24/24 on the Epworth Sleepiness Scale), frequent nocturia and back pain. The patient observed that sleeping in a reclining chair alleviated his back pain and nocturnal awakenings due to choking.
On physical examination his BMI was 36 kg/m2 and his neck circumference was 42 cm.
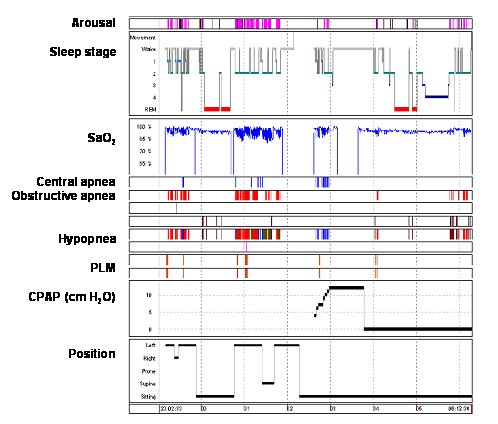
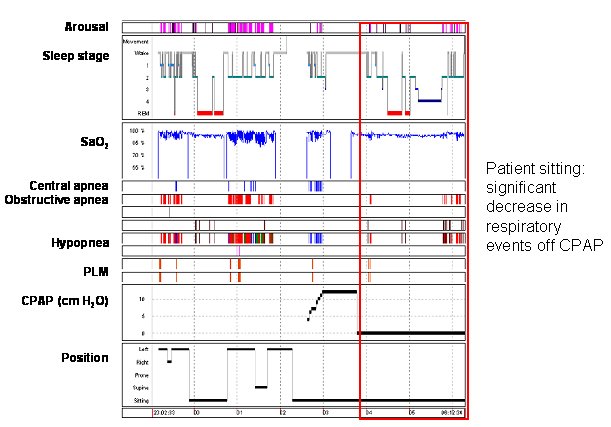
Based on the hypnogram what intervention best controlled this patient’s obstructive respiratory events?
Sleeping in the upright position.
During the first three hours, the sleep hypnogram displays obstructive apneas and hypopneas with desaturations and micro-arousals in both the lateral and supine positions. No respiratory events were recorded during REM sleep, although the patient had moved to a chair to sleep. His overall AHI was 58 events/h.
Although minimal obstructive respiratory events were observed with the patient in the sitting position, CPAP titration was initiated while he remained sitting. Recurrent central apneas with arousals were observed and CPAP was not tolerated beyond 3:40 AM. For the remainder of the night, there was a decrease in respiratory events observed while he slept seated (see red-boxed area in figure).
While lateral to supine positional sleep apnea is well recognized, relief of obstructive events in the sitting position is less appreciated. Several mechanisms may explain the decreased severity of sleep apnea from the supine to the seated position. Cephalometric data suggest a significant increase in the antero-posterior dimension of the airway at the level of the velopharynx and the oropharynx when moving from the supine to the seated position (1, 2). In addition, upper airway collapsibility measurements (Pcrit) markedly decrease from a supine position to a 30 degree incline, decreasing susceptibility to recurrent obstructive respiratory events (3). Furthermore, upright resting lung volumes (functional residual capacity; FRC) are increased compared to the supine position and can potentially result in two effects. First, increased lung volumes decrease airway collapsibility (4) and decrease CPAP requirements (5), presumably through increases in tracheal traction (6). Furthermore, increased FRC is correlated with increased oxygen stores, which may improve central respiratory control stability and recurrent disordered breathing events (7, 8).
References
- Tsuiki S et al. Supine-dependent changes in upper airway size in awake obstructive sleep apnea patients. Sleep Breath 2003; 7:43-50.
- Battagel JM, et al. Postural variation in oropharyngeal dimensions in subjects with sleep disordered breathing: a cephalometric study. Eur J Orthod 2002; 24:263-276.
- AM Neill, et al. Effects of sleep posture on upper airway stability in patients with obstructive sleep apnea. Am J Respir Crit Care Med 1997; 155: 199-204.
- Tagaito Y, et al. Lung volume and collapsibility of the passive pharynx in patients with sleep-disordered breathing. J Appl Physiol. 2007 Oct;103:1379-85.
- Heinzer RC, et al. Lung volume and continuous positive airway pressure requirements in obstructive sleep apnea. Am J Respir Crit Care Med. 2005; 172:114-7.
- Rowley JA, et al. Effect of tracheal and tongue displacement on upper airway airflow dynamics. J Appl Physiol 1996; 80: 2171-8.
- Younes M, et al. Chemical control stability in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 2001; 163: 1181–1190.
- Younes M. Contributions of upper airway mechanics and control mechanisms to severity of obstructive apnea. Am J Respir Crit Care Med 2003; 168:645–658.