Contributed by Fiona Healy, MBBCh, Division of Pulmonary Medicine, Children’s Hospital of Philadelphia. Carole L. Marcus, MBBCh, Sleep Center, Children’s Hospital of Philadelphia.
A 16 year old boy with a mitochondrial disorder, central and obstructive sleep apnea, kyphoscoliosis and right hemiparesis following a cerebrovascular accident was referred for a titration study of his current non-invasive ventilation settings. The patient required nocturnal ventilation only with bilevel positive airway pressure (BLPAP). In a previous study (15 months prior) the patient was titrated to his current home settings of 14/10 cm H2O in the spontaneous timed (ST) mode with a rate of 14 breaths per minute (bpm) on room air.
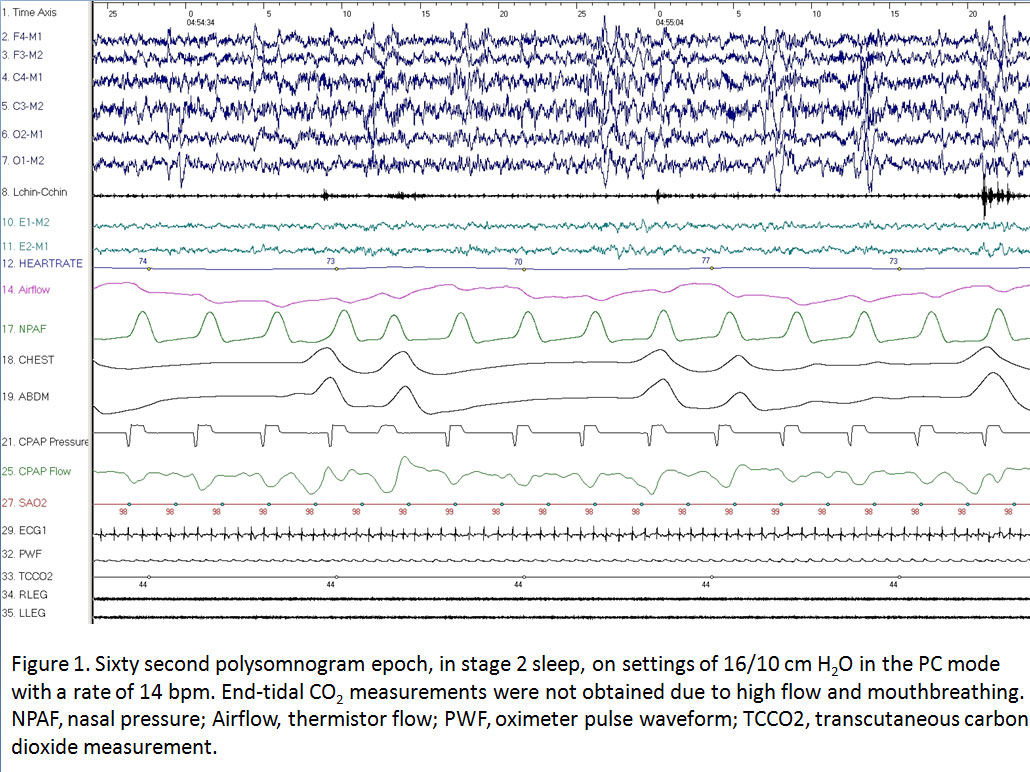
The study was initiated on the patient’s home settings using a BLPAP machine with a nasal cannula interface. Mouth breathing was noted intermittently throughout the study. The patient was titrated to final settings of 16/10 cm H2O in the pressure control (PC) mode with a rate of 14 bpm on room air.
Questions:
1. What abnormality is shown on this polysomnogram epoch (figure 1), taken from when the patient was at the final titration settings mentioned above?
2. What factors could have contributed to this finding?
3. What interventions could be performed to eliminate this abnormality?
Answers:
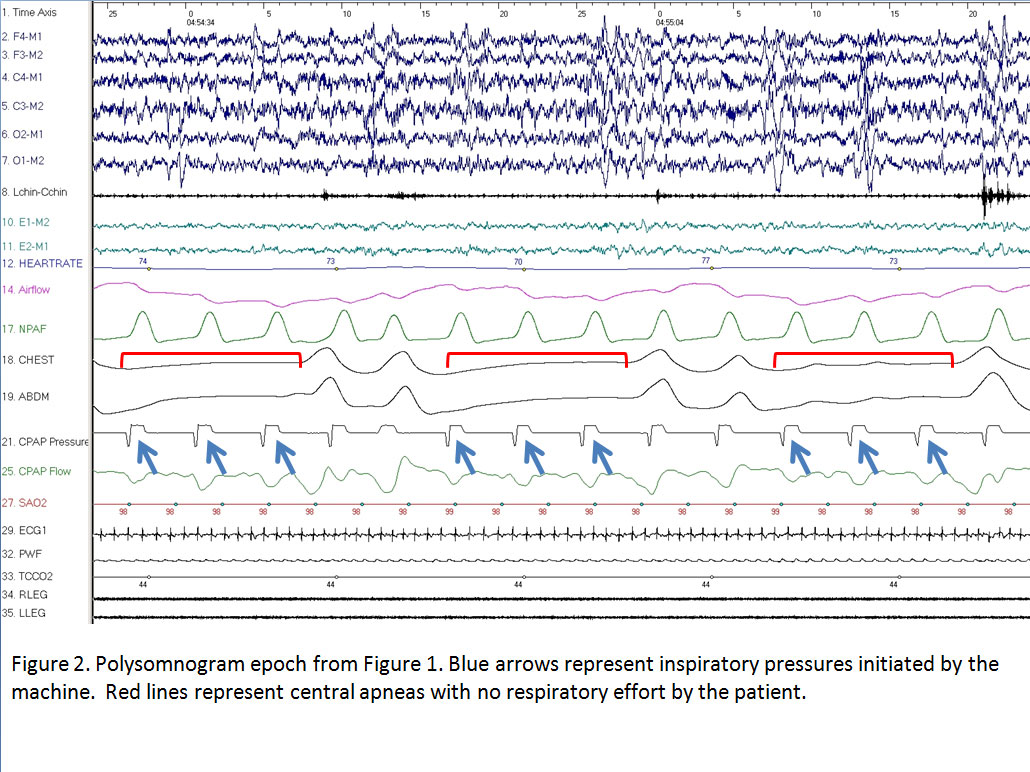
1. The breaths are adequately initiated by the ventilator but because of a short inspiratory time (Ti) the breaths are cycled off before there is time for the delivered pressures to move the chest wall, resulting in central apneas (figure 2).
2. The short Ti and mouth breathing.
3. Adjust the set Ti on the ventilator. Use of a chinstrap, full-facemask or combined nasal and oral interface would treat mouth breathing.
Discussion:
The initial approach to treating patients with neuromuscular weakness with sleep disordered breathing, whether due to central apnea, obstructive apnea, or gas exchange abnormalities due to hypoventilation, is to apply noninvasive ventilation during sleep, titrated to appropriate settings.1 Ventilation modalities currently used in this population include BLPAP in spontaneous mode (breaths initiated by the patient only, with no back up rate), ST mode (a backup rate is available to deliver pressure if the patient does not initiate a breath within a set time window), timed mode (Ti and respiratory rate are fixed) and PC mode (similar to ST mode except that all breaths are machine cycled).2, 3
In this study, the sleep technologist switched the patient from ST mode (baseline settings) to PC mode in an attempt to address the loss of delivered pressure due to mouth breathing. However, a more appropriate response would have been to use a chinstrap or full facemask. This could have resolved the mouth breathing and subsequently improved pressure delivery and chest wall movement without having to increase pressures or switch to PC mode. When considering the use of a full facemask however, it is important to be aware of the risk of aspiration, which can be increased in patients with neuromuscular disorders.
During this titration study the patient was switched from ST to PC mode with a set respiratory rate and Ti. In this situation the machine initiates and delivers breaths at a set pressure and rate. Any additional spontaneous breaths taken by the patient, between the machine initiated breaths, are not supported by pressure from the machine. In PC mode, the ventilator cycles off the breaths when the pressure is delivered for a set Ti. In this sample, the Ti was set at 0.3 seconds which is extremely short for the patient’s own respiratory rate of 12bpm. For a normal inspiratory:expiratory ratio of 1:2, this respiratory rate should allow inspiratory time of 1.66 seconds (vs 0.3 seconds) and an exhalation time of 3.34 seconds. The short Ti in this case could not sustain the delivered breaths for long enough to move the chest wall with resulting central apneas (Figure 2, red lines). The blue arrows in figure 2 clearly represent breaths initiated by the ventilator and not the patient as there is no evidence of respiratory effort to initiate the breaths in either the chest or abdominal leads on the patient.
This example demonstrates the problems faced when the Ti is not set appropriately to the patient’s ventilatory needs. The physician and sleep technologist must be aware of the default settings on the ventilators that they are using to provide accurate titration information. A specific area of concern is for patients with neuromuscular weakness with low inspiratory flow rates who cannot trigger the pressure support features of current ventilators. The pediatric neuromuscular population, in particular, is at high risk for both triggering and cycling problems as the algorithms in these machines are designed for adults. To date, there are no BLPAP machines approved by the Food and Drug Administration for use in children under 7 years old and weighing less than 40lbs. In some cases, if left at default settings, the Ti is too long for younger children and therefore the required inspiratory pressure is not met before the child cycles into expiration.4
Although we were able to obtain accurate transcutaneous carbon dioxide (CO2) measurements during the study, we were unable to obtain end tidal CO2 monitoring due to significant mouth breathing by the patient. The capnography tracing would have been helpful in this case because it would specifically represent the flow from the patient alone while the nasal pressure and CPAP flow tracings represent the combination of the patient and machine air flow. This differentiation would help to identify exactly what support was delivered to the patient by the ventilator and what effort they were generating for themselves.
This case highlights the importance of reviewing the intrinsic algorithms of the ventilator used and adjusting the default settings to suit the patient’s needs during a titration study. There is clearly a need for machines that can specifically address the ventilatory needs of pediatric patients with neuromuscular disorders.
References
1. Arens R, Muzumdar H. Sleep, sleep disordered breathing, and nocturnal hypoventilation in children with neuromuscular diseases. Paediatr Respir Rev. 2010;11:24-30.
2. Berry RB, Chediak A, Brown LK, et al. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6:491-509.
3. www.respironics.com/UserGuides/UserGuideBiPAPSynchrony.pdf
4. Liner LH, Marcus CL. Ventilatory management of sleep-disordered breathing in children. Curr Opin Pediatr. 2006;18:272-276.