Contributed by Carles Gaig, Joan Santamaria, Neurology Service and Multidisiciplinary Sleep Disorders Unit, Hospital Clinic of Barcelona; Barcelona, Catalonia, Spain
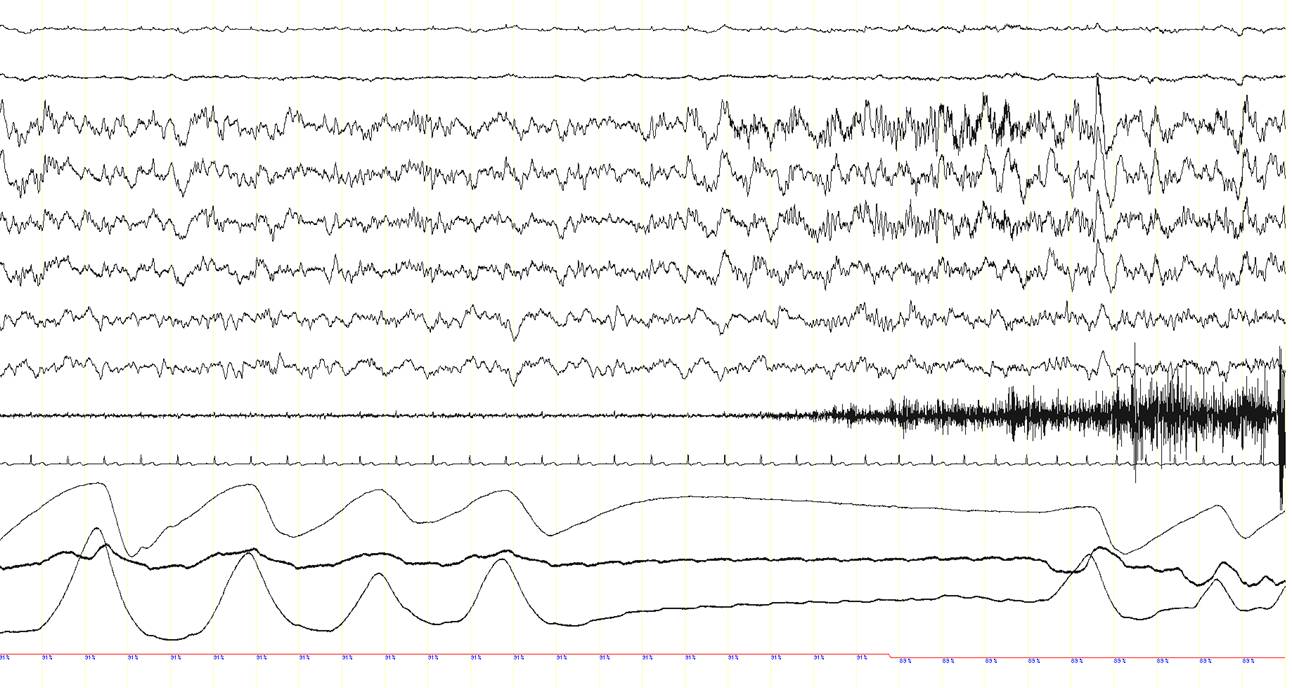
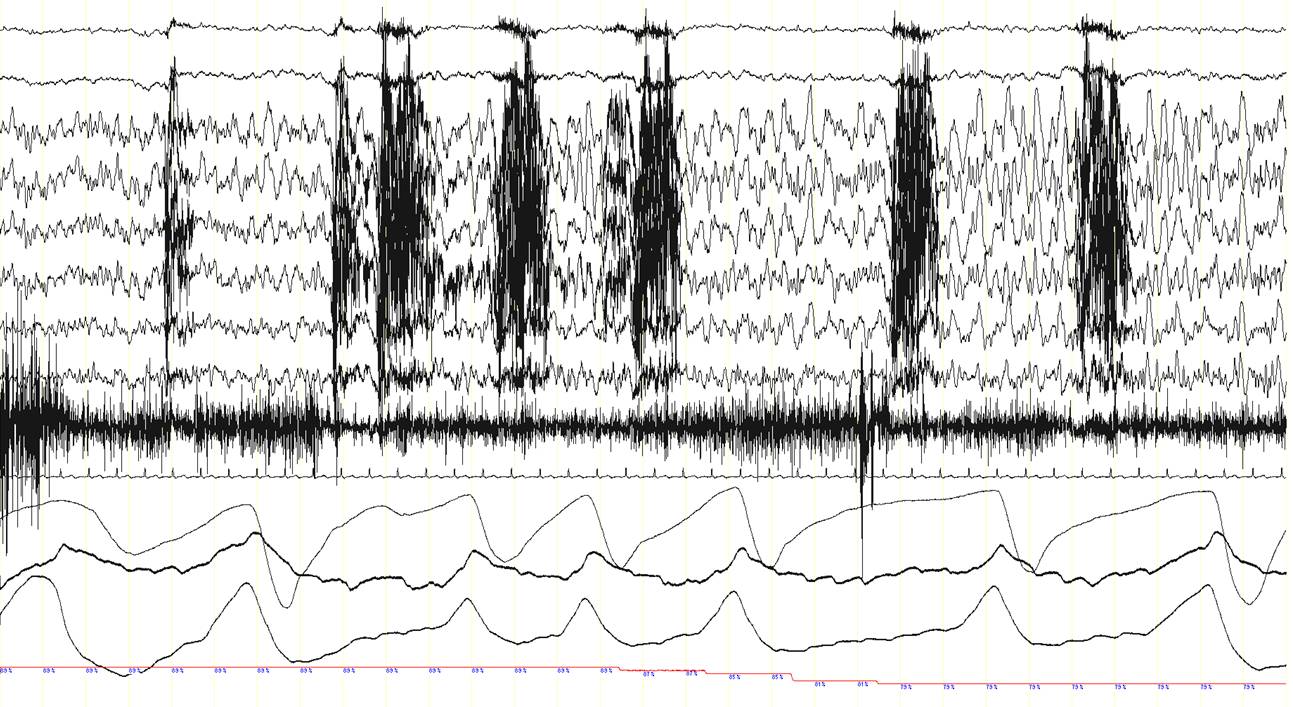
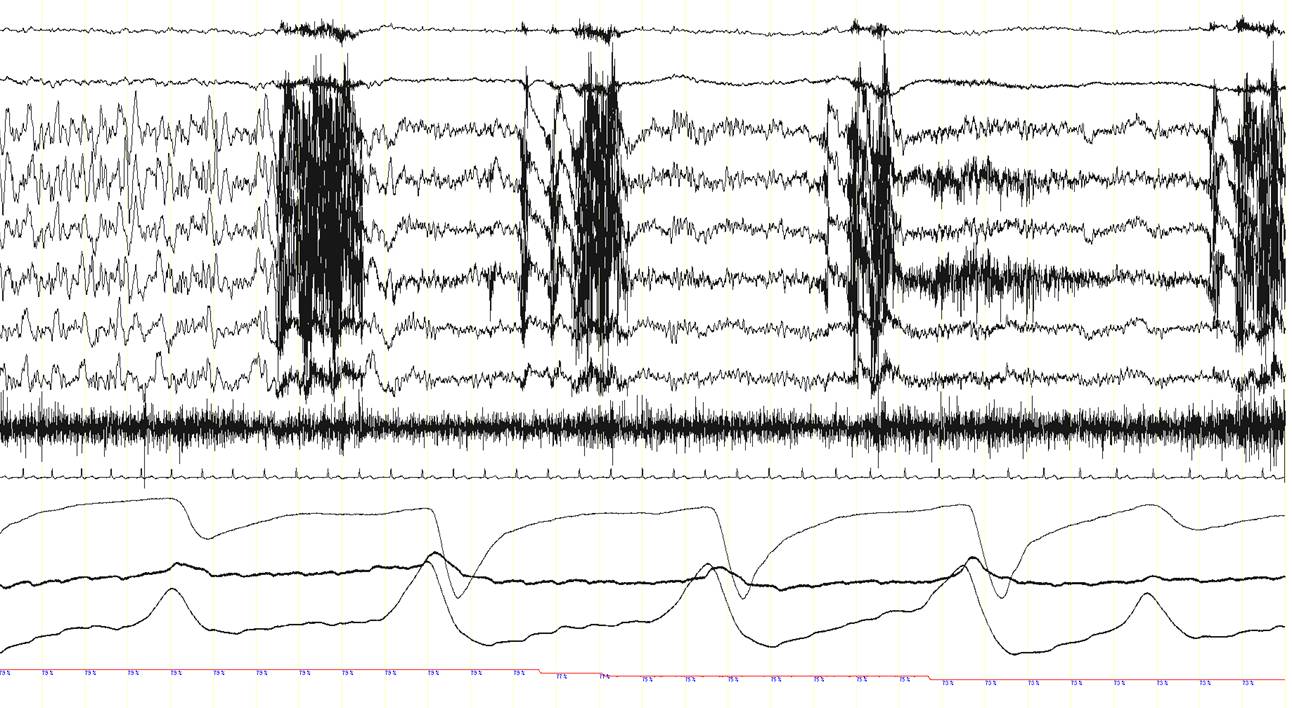
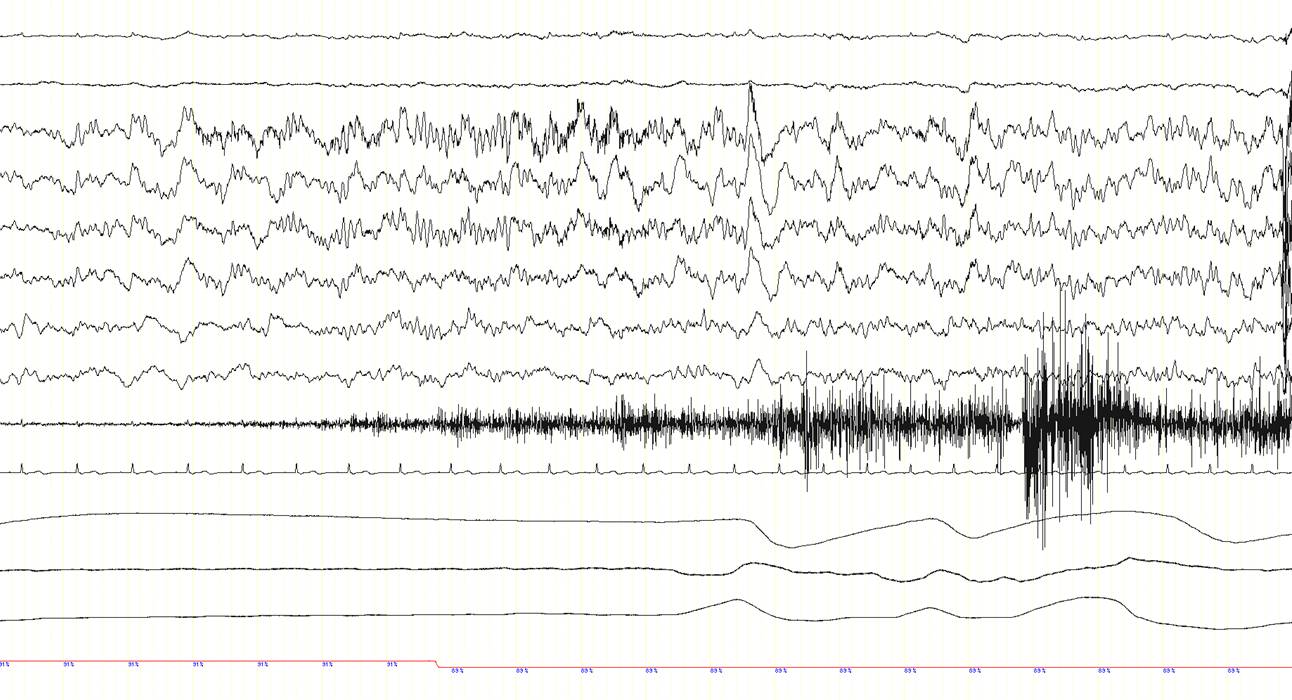
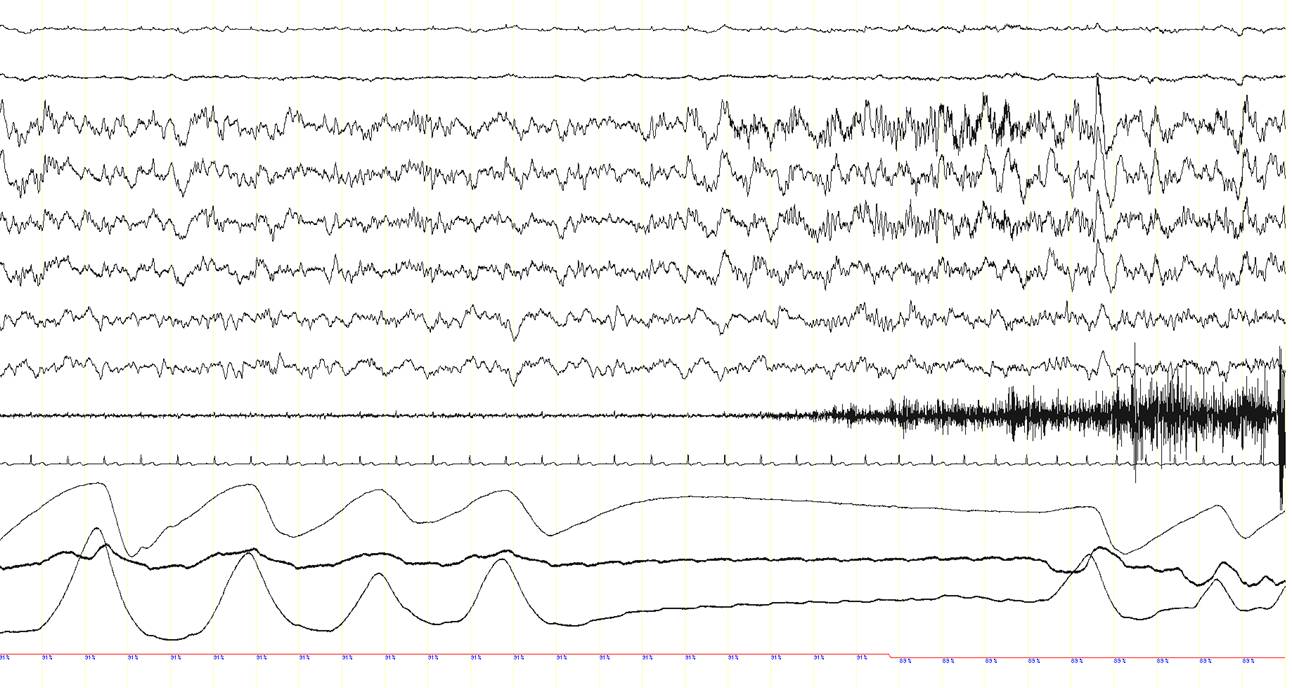
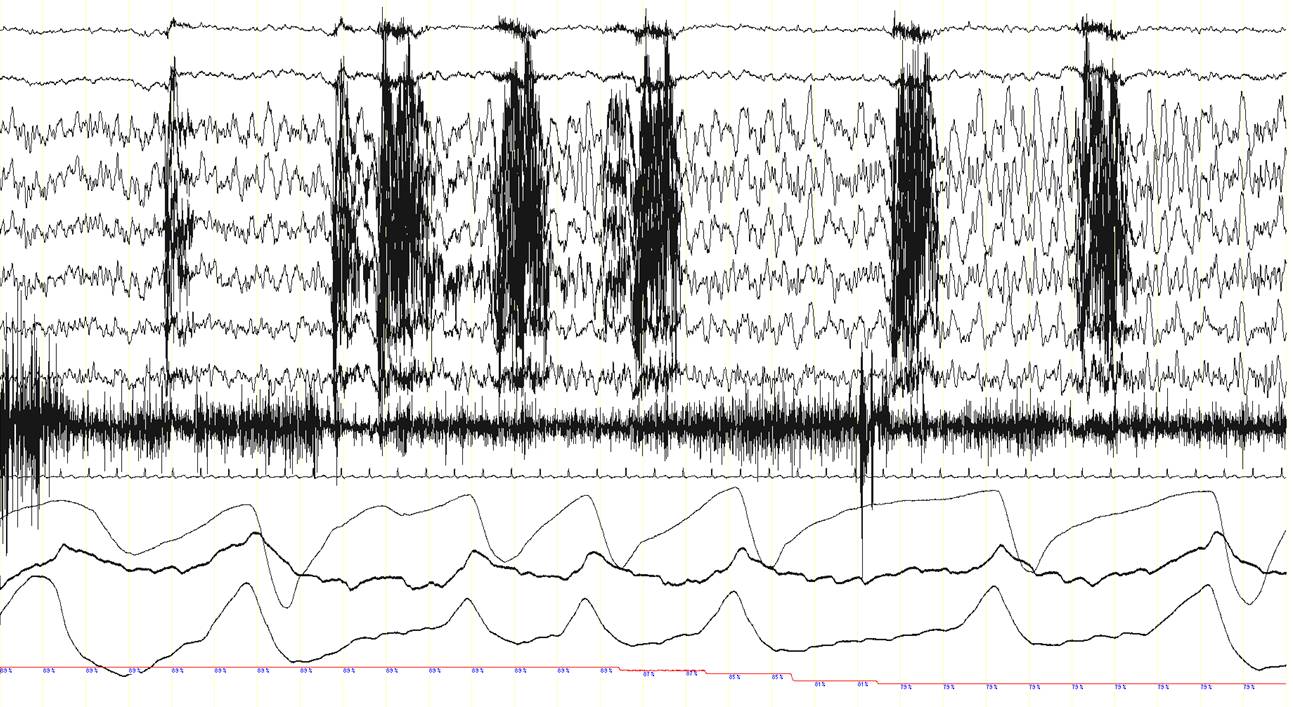
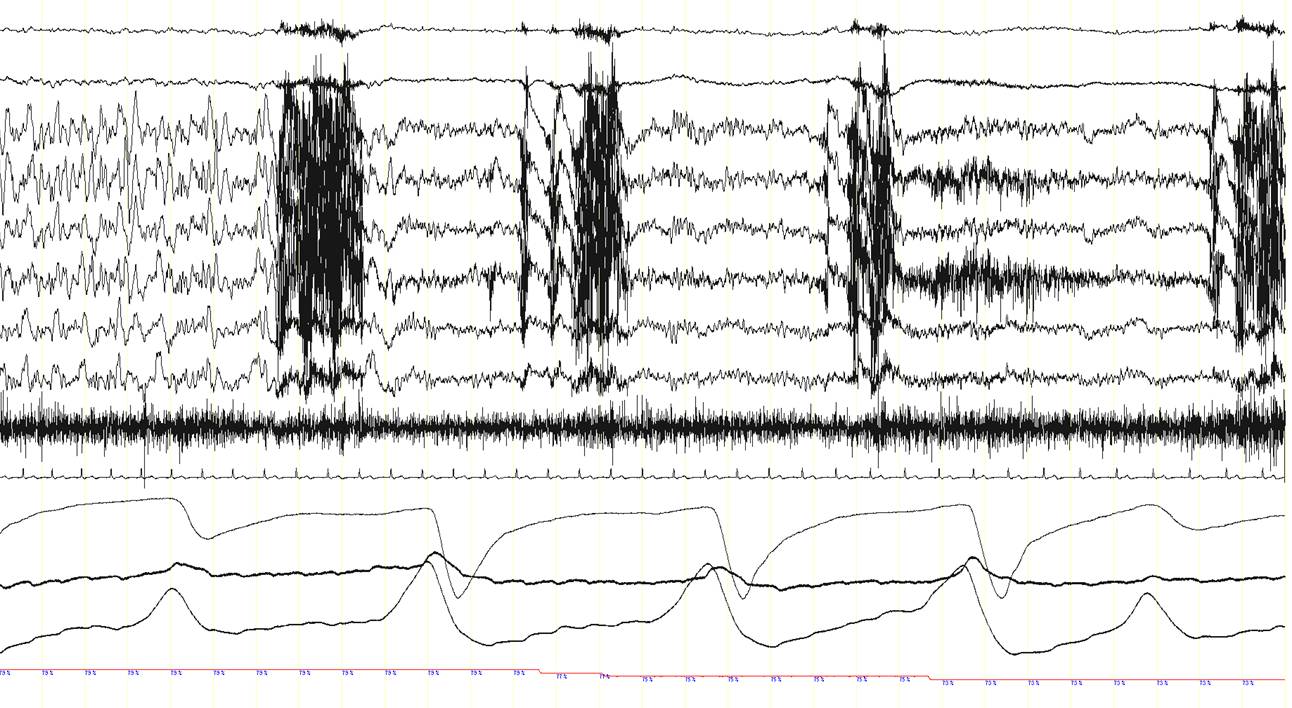
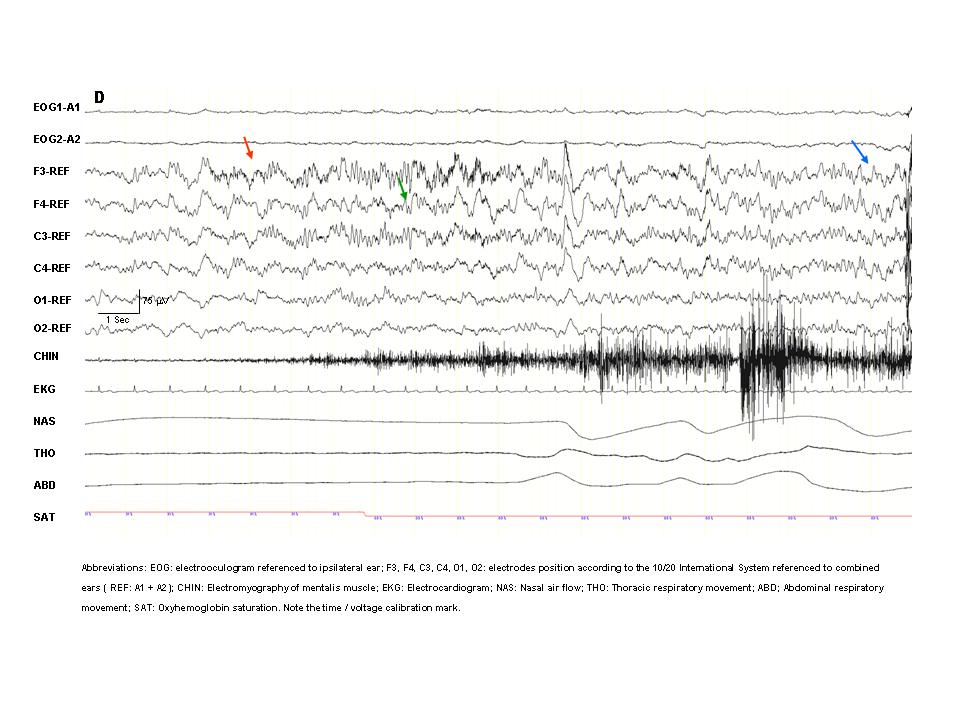
A 63 year-old man was diagnosed with obstructive sleep apnea syndrome because of habitual heavy snoring with breathing pauses during sleep, occasional awakenings and mild excessive daytime somnolence. The patient also complained of recurrent episodes of sudden dizziness, pallor, sweating, and sometimes pain in the right shoulder, either awake or during sleep. An electroencephalography (EEG), brain CT scan and cardiac exercise stress test revealed normal findings and the nature of these episodes had remained elusive. A baseline polysomnographic (PSG) study showed frequent obstructive sleep apneas, particularly in the supine position (apnea-hypopnea index in this position: 33/hour; not shown here). A subsequent continuous positive airway pressure (CPAP) titration PSG study was performed. With a CPAP pressure of 7 cm H2O obstructive events were well-controlled. Suddenly, however, the patient presented an apnea (panel A, between arrows) with a change in the EEG signals. This is shown in the three consecutive 30-second epochs (panel A, B and C). In panel D, a 20-second epoch of the event is shown. Can you describe what is happening here?
Click on images to enlarge.
This patient had a focal seizure with secondary generalization starting with an ictal central apnea.
DISCUSSION
Note the presence of epileptogenic activity on the EEG channels just after the onset of the central apnea while the patient is in NREM sleep (N2). A rhythmic 8-9 Hz EEG activity is recorded in the left frontal area (red arrow, F3-REF), which rapidly spreads over the rest of the hemisphere and to the contralateral side (green arrow), and progressively increases in amplitude and decreases in frequency to theta (4-5 Hz) and finally delta ranges (2-3 Hz) (blue arrows). This ictal EEG rhythmic activity lasted approximately 1 minute (end of the ictal rhythm: red arrow in the third epoch; panel C). Remarkably, during this seizure with an initial ictal central apnea, oxyhemoglobin saturation dropped to 73%. The patient also presented repetitive chewing movements (see the artefact caused by masticatory movements in the EEG channels; red asterisks), but overt convulsions or other abnormal movements or behaviours were not recorded. The patient was unaware of this seizure and did not recall any event during the night the following morning.
This event prompted a review of the clinical history. During the last four years the patient had presented 4-5 times a month, while sleeping, episodes of sudden awakening with dizziness, pallor, sweating, and sometimes pain in the right shoulder. These attacks lasted 10 to 20 second and consciousness was partially preserved: the patient felt a little bit confused but he could remember what happened. He had occasionally similar daytime attacks (1-2 times a month), while awake but he had never received a diagnosis of epilepsy. Brain MRI was normal. A routine EEG showed occasional interictal epileptiform abnormalities (spikes and sharp waves) over the left frontal area, and an episode of ictal rhythmic activity over this brain area without clinical manifestations was recorded (subclinical seizure).
In addition to obstructive sleep apnea, cryptogenic frontal lobe epilepsy was diagnosed. Therapy with oxcarbamazepine 600 mg twice daily was introduced and obstructive sleep apnea was successfully treated with CPAP with a dramatic reduction in seizure frequency (1-2 mild nocturnal seizures a month and no seizures during daytime).
The present case illustrates several points: first, apneic events may be caused by epilepsy, due to the associated changes in autonomic function, such as in cardiac or breathing rhythm, occurring during the seizure (1). Ictal apnea is usually central as result of reduced central breathing drive, but obstructive events can rarely occur (1, 2). Nocturnal seizures often arise from frontal lobe and typically occur during NREM sleep (N2) (3). Second, epilepsy and obstructive sleep apnea may coexist, given the relatively high prevalence of both disorders. Recent studies, however, suggest that obstructive sleep apnea could be more common than expected in patients with refractory epilepsy (4). The association of epilepsy and obstructive sleep apnea can potentially aggravate both disorders. Obstructive sleep apnea could worsen epilepsy and treating sleep apnea might improve it (5). On the other side, epilepsy could potentially increase the number of apneic events in patients with obstructive sleep apnea. Third, the reduced EEG montage used in a PSG may give clinically relevant information, even in patients with an apparently “typical” sleep apnea.
References
- Nashef L, Walker F, Allen P, Sander JW, Shorvon SD, Fish DR. Apnoea and bradycardia during epileptic seizures: relation to sudden death in epilepsy. J Neurol Neurosurg Psychiatry 1996; 60:297-300.
- Blum AS, Ives JR, Goldberger AL, Al-Aweel IC, Krishnamurthy KB, Drislane FW, Schomer DL. Oxygen desaturations triggered by partial seizures: implications for cardiopulmonary instability in epilepsy. Epilepsia 2000; 41:536-541.
- Tinuper P, Provini F, Bisulli F, Vignatelli L, Plací G, Vetrugno R, Montagna P, Lugaresi E. Movement disorders in sleep: Guidelines for differentiating epileptic from non-epileptic motor phenomena arising from sleep. Sleep Med Rev 2007; 11:255-267.
- Chihorek AM, Abou-Khalil B, Malow BA. Obstructive sleep apnea is associated with seizure occurrence in older adults with epilepsy. Neurology 2007; 69:1823-1827.
- Vaughn BV, D’Cruz OF, Beach R, Messenheimer JA. Improvement of epileptic seizure control with treatment of obstructive sleep apnea. Seizure1996; 5:73-78.
Click on images to enlarge.