Contributed by Abhishek Biswas M. D., Richard B. Berry M.D., Peruvemba S. Sriram M.D., Ashish Prasad M.D. University of Florida, Department of Pulmonary and Critical Care Medicine, 1600 SW Archer Rd, Gainesville, Florida-32610 Corresponding Author: Abhishek Biswas, Fellow, University of Florida, Department of Pulmonary and Critical Care Medicine, 1600 SW Archer Rd, Gainesville, Florida-32610. Email: abiswas@ufl.edu Tel: 352-273-8734 Fax: 352-273-9154
Case Vignette
A 61-year-old man presented with increasingly bothersome palpitations that awoke him at night but did not occur during the day. His wife reported that he would frequently snore at night and appeared to stop breathing at times. The patient denied daytime sleepiness, chest pain, pre-syncope or syncope symptoms. His Epworth scale was 7/24. He had a history of hypertension and benign prostatic hyperplasia, but was otherwise well.
Physical examination revealed a healthy appearing male with a body mass index (BMI) of 24 kg/m2 and a Mallampatti II airway. Cardiac examination revealed a regular heart rate of 68 beats per minute with normal heart sounds and no murmurs or rubs. The remainder of the physical examination was normal.
A diagnostic polysomnogram, performed to evaluate the patient for obstructive sleep apnea (OSA), revealed a total sleep time of 5.5 hours, an overall apnea-hypopnea index (AHI) of 9.1 events per hour, a non-REM AHI of 5.8 events per hour, and a REM AHI of 24.4 events per hour. The minimum oxyhemoglobin saturation during NREM sleep was 85% and during REM sleep was 92%. ECG abnormalities were noted only during REM sleep, during periods with (Figure 1) and without obstructive respiratory events (Figure 2). Under the care of a cardiology consultant, the patient underwent electrophysiological event monitoring. Complete heart block was observed only during times when he reported being asleep.
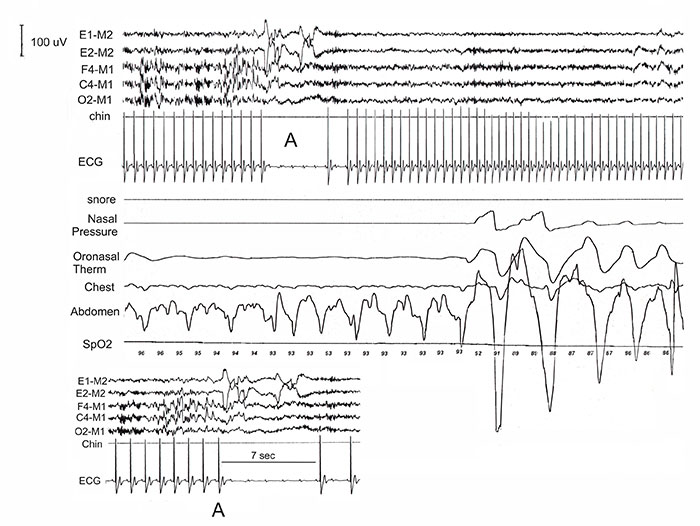
Figure 1: A 60-second tracing showing the end of a long obstructive apnea with a blow up of the area of interest (A). During the event a transition from stage N2 (sleep spindles visible) to REM sleep (rapid eye movements) was noted. At the time of transition to REM sleep the ECG shows complete heart block with a ventricular pause of 7 seconds. Arousal from sleep is noted immediately after the period of complete heart block
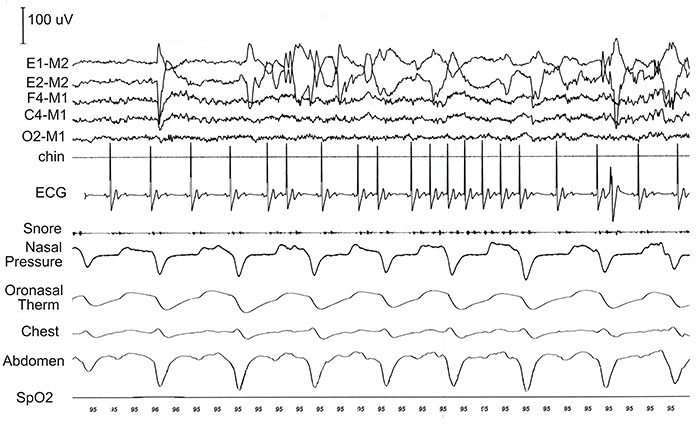
Figure 2: A 30-second epoch recorded during the same encounter demonstrates phasic REM associated second-degree heart block without any evidence of apnea/hypopnea during this period.
The patient was initiated on auto-titrating CPAP (APAP) with a minimum pressure of 8 cm of water and a maximum pressure of 12 cm of water. Data download from the APAP device revealed an AHI of 2.3 events per hour and excellent adherence. However, the patient reported persistent symptoms during sleep. A cardiac event-monitor recording during APAP after one week of PAP treatment revealed persistent sleep-related symptomatic bradycardia (Figure 3).
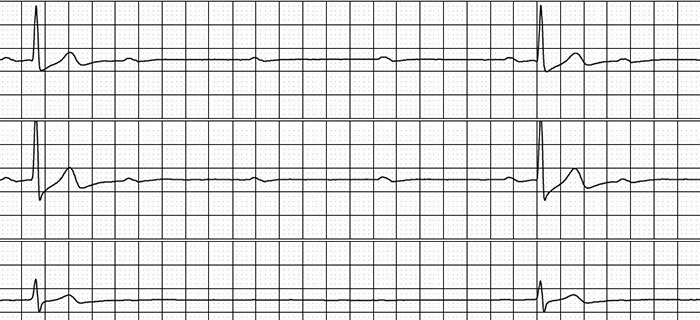
Figure 3: An event recorder tracing while the patient slept with APAP still shows persistent bradycardic episodes due to complete heart block after one week of treatment.
Questions
-
What is the likely diagnosis?
-
What is the best treatment option?
Discussion
Arrhythmias during sleep are not uncommon. They can range from benign self-terminating abnormalities to potentially lethal ventricular tachyarrhythmias as seen in patients with congestive heart failure. Tachyarrhythmias during sleep may also signify the presence of underlying obstructive sleep apnea, usually of at least moderate severity (1). Bradyarrhythmias, such as atrioventricular block, sinus pauses, and asystole have also been described in OSA (2). In a study of 400 patients with OSA, 48% had documented cardiac arrhythmias, including sinus arrest in 11% and second-degree atrioventricular block in 8% (3). The most common form of bradycardia noted with OSA is termed cyclic variation in heart rate (CVHR) (4). It is characterized by progressive bradycardia during the apneic period followed by periods of tachycardia.
Bradycardia was observed in our patient exclusively during REM sleep. Obstructive sleep apnea was also seen primarily during REM sleep. While it is possible the observed atrioventricular block was due to obstructive sleep apnea, the persistence of complete heart block with successful treatment of OSA as inferred by the patient’s APAP download data and the presence of second degree heart block during REM sleep in the absence of obstructive respiratory events (Figure 2) suggested that the heart block was likely to be secondary to REM sleep rather than OSA itself.
This sleep stage specific arrhythmia has been referred to as REM-related bradyarrhythmia syndrome, first described by Guilleminault and colleagues in 1984 (5). Polysomnographic testing demonstrates transient sinus arrest or 3rd degree atrioventricular block with ventricular arrest during phase REM sleep independent of sleep-disordered breathing.
REM sleep-related bradyarrhythmia syndrome is a rarely reported phenomenon with only a handful of case reports. Patients are commonly middle aged and otherwise healthy without OSA. A clear explanation for REM-related bradyarrythmia is still elusive. A balance between sympathetic and parasympathetic tone determines heart rate in sleep and during periods of wakefulness. These autonomic components are regulated by sleep stage cycle, body posture, sleep apnea and arousals (6).
High amplitude bursts of sympathetic activity with inhibition of parasympathetic discharge are more common with REM-sleep resulting in autonomic instability and tachycardia (7). Abnormal autonomic regulation of cardiac rhythm in the form of an exaggerated vagal tone during REM sleep is hypothesized to be responsible for REM sleep related bradyarrhythmias. Occasional heart rate decelerations associated with phasic REM sleep events have also been described in healthy asymptomatic adults leading to bradycardia (8). Thus, although REM sleep is suspected to be a sympathetic-predominant phasic event, there are studies demonstrating variability in the balance between sympathetic to parasympathetic discharges.
The optimal treatment for REM-related bradyarrhythmia syndrome remains unknown. Treatment options include pharmacologic therapy utilizing the anticholinergic effect of medications such as atropine and tricyclic antidepressants (9, 10). Surgical vagotomy has been reported to blunt REM-related sinus arrest in animal models (9, 10). Majority of patients who have had sinus-arrests and complete heart block have had permanent pacemaker implantation (3). Prophylactic pacing is somewhat controversial. The validity of the assumption that REM-related sinus arrest or atrioventricular block predisposes to sudden nocturnal cardiac death is unproven. There are published cases of those who have done well without the need for a pacemaker.
Answers
-
What is the likely diagnosis?
A diagnosis of REM-related bradyarrhythmia syndrome is favored -
What is the best treatment option?
Optimal treatment remains unknown but consideration of permanent pacemaker implantation is suggested for symptomatic phasic-REM associated heart block.
Follow-Up
A permanent pacemaker was implanted for suspected phasic-REM associated bradyarrhythmia syndrome. With the pacemaker in place, the patient has not experienced any recurrence of nocturnal palpitations.
References
-
Gula L, Krahn A, Skanes A, Yee R, Klein G. Clinical relevance of arrhythmias during sleep: guidance for clinicians. Heart. 2004;90(3):347-52.
-
Rossi VA, Stradling JR, Kohler M. Effects of obstructive sleep apnoea on heart rhythm. European Respiratory Journal. 2013;41(6):1439-51.
-
Guilleminault C, Connolly SJ, Winkle RA. Cardiac arrhythmia and conduction disturbances during sleep in 400 patients with sleep apnea syndrome. The American journal of cardiology. 1983;52(5):490-4.
-
Shepard Jr JW. Hypertension, cardiac arrhythmias, myocardial infarction, and stroke in relation to obstructive sleep apnea. Clinics in chest medicine. 1992;13(3):437-58.
-
Janssens W, Willems R, Pevernagie D, Buyse B. REM sleep-related brady-arrhythmia syndrome. Sleep and Breathing. 2007;11(3):195-9.
-
Burgess HJ, Trinder J, Kim Y, Luke D. Sleep and circadian influences on cardiac autonomic nervous system activity. American Journal of Physiology-Heart and Circulatory Physiology. 1997;273(4):H1761-H8.
-
Snyder F, Hobson JA, Morrison DF, Goldfrank F. Changes in respiration, heart rate, and systolic blood pressure in human sleep. Journal of Applied Physiology. 1964;19(3):417-22.
-
Taylor WB, Moldofsky H, Furedy JJ. Heart rate deceleration in REM sleep: an orienting reaction interpretation. Psychophysiology. 1985;22(1):110-5.
-
Guilleminault C, Pool P, Motta J, Gillis AM. Sinus arrest during REM sleep in young adults. New England Journal of Medicine. 1984;311(16):1006-10.
-
Otsuka K, Ikari M, Ichimaru Y, Saito H, Kawakami T, Kaba H, et al. Experimental study on the relationship between cardiac arrhythmias and sleep states by ambulatory ecg‐EEC monitoring. Clinical cardiology. 1986;9(7):305-13.



