Contributed by Contributed by Lourdes M. DelRosso, M.D., Romy Hoque, M.D., Division of Sleep Medicine, Department of Neurology, Louisiana State University Health Sciences Center, Shreveport LA
In Brief:
A woman with multiple medical problems was found to have severe sleep disordered breathing. Further work up revealed an underlying genetic condition, which may contribute to her sleep disorder.
A 56-year-old African American presented for evaluation of snoring and excessive daytime sleepiness. She had a history of hypertension; hyperlipidemia; glaucoma with normal visual acuity bilaterally; ectopic pelvic kidney; severe external auditory canal atresia bilaterally; conductive hearing loss bilaterally with conduction hearing aids in place; and a limited range of neck motion. Daily medications included amlodipine 2.5 mg, atorvastatin 40 mg, lisinopril-hydrochlorothiazide 20-12.5mg.
Her height was 4 feet 11 inches, weight 144 pounds, body mass index of 29.1. She was alert, pleasant and able to provide a clear history. Her neck was short, with limited extension. Posterior hairline was low, and she had external auditory canal malformation (Figure 2C). Oral airway was Mallampatti IV, tonsils 2+. Lungs were clear to auscultation. Neurologic exam was normal except that strength was 4/5 for shoulder abduction bilaterally, right elbow flexion, and hip flexion bilaterally. Mirror movements (voluntary/active movements of one extremity that are mimicked by involuntary/passive movements in the opposite extremity) were not observed.
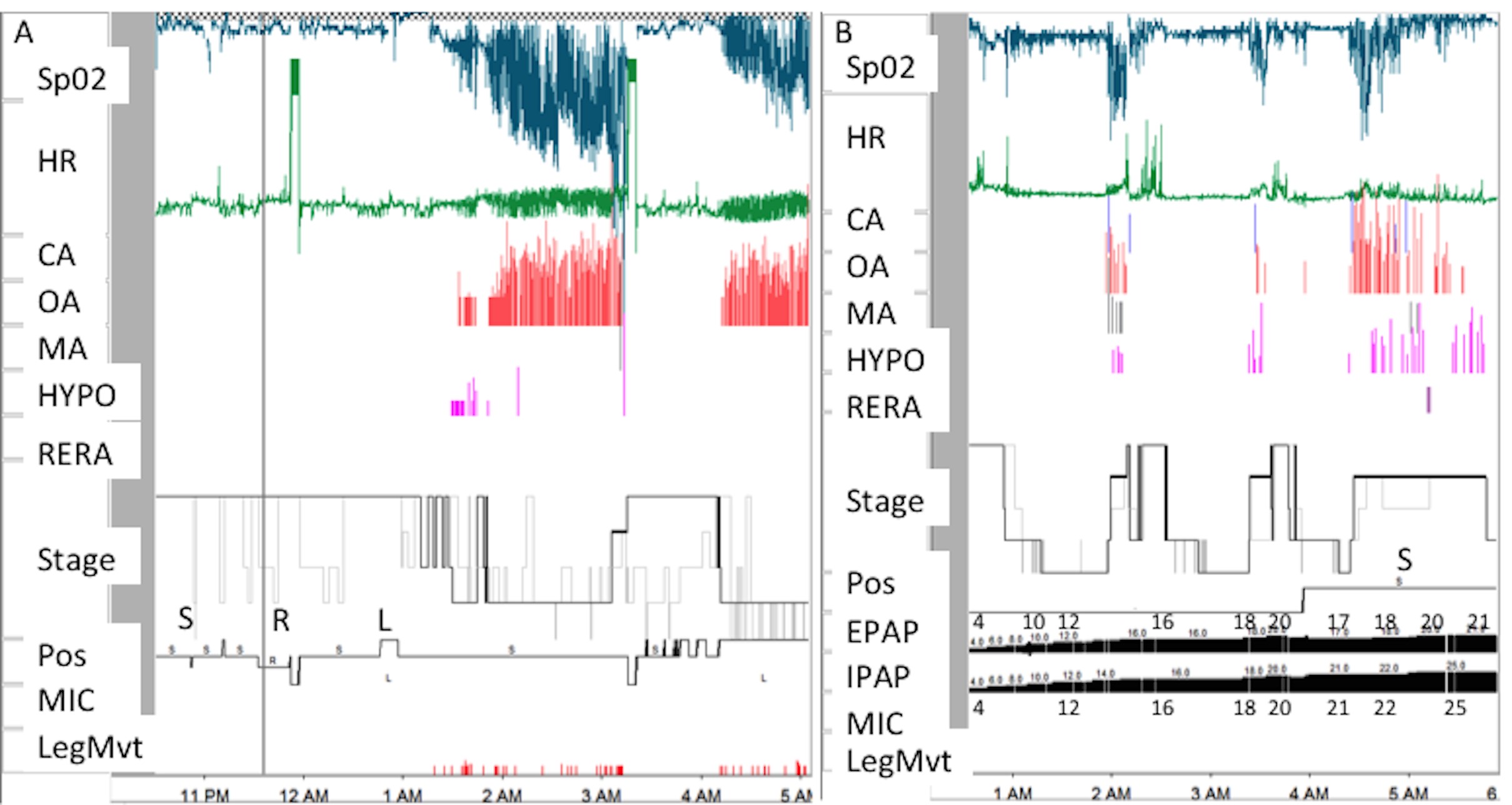
Her Epworth Sleepiness Scale Score was 13/24. Diagnostic polysomnogram showed severe sleep disordered breathing with an apnea hypopnea index of 98 events her hour. The apnea events were predominantly obstructive (Table 1). A positive airway pressure titration polysomnogram was performed and bilevel positive airway pressure of 25/21 cmH2O was recommended (Figure 3).
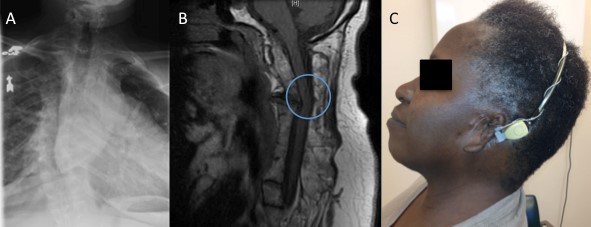
Given the severity of her sleep disordered breathing, a neck radiograph was ordered. On lateral view, fusion of cervical vertebrae C1-C3 was noted (Figure 1). A chest radiograph showed dextro-scoliosis without thoracic vertebral fusion (Figure 2A). Magnetic resonance imaging (MRI) of the cervical spine revealed fusion of the first three cervical vertebrae with degenerative changes throughout the cervical vertebrae, protrusion into the cervical canal, and reversal of normal cervical curvature (Figure 2B). Arnold-Chiari malformation was not seen. Spinal cord signal intensity was normal. MRI of the brain, and brainstem was normal.
On the basis of the physical examination and radiographic findings, a diagnosis of Klippel-Feil syndrome (KFS) was established.
A transnasal esophagoscopy was performed to further evaluate her airway. The standard endoscope was passed with ease through the mouth under direct visualization to the hypopharynx. Pulse oximetry revealed abrupt oxyhemoglobin desaturation when the scope was advanced into the cryopharyngeaus to the level of the white arrow in Figure 1. A pediatric endoscope was then used and passed without difficulty. No further abnormalities were encountered.
On spirometry, she had a limited ability to blow out for 6 consecutive seconds. Forced vital capacity (FVC) was 1.05 liters (48 % of predicted). Forced expiratory volume in one second (FEV1) was 0.88 liters (51% of predicted). FEV1/FVC percentage was 84% (106% of predicted). These results are suggestive of with restrictive chest disease, likely related to her scoliosis. Room air arterial blood gasses were consistent with a chronic compensated respiratory acidosis, with a pH of 7.43, pC02 of 50 mmHg, pO2 of 69 mmHg, and HCO3 of 31.1 mmol/L.
An echocardiogram revealed normal right and left ventricular function with left ventricular ejection fraction of 60%. Nuclear stress test did not show evidence of inducible ischemia.
Figure 1: Lateral radiograph of this patient’s head and neck showing a cervical spinal deformity (white arrow) attributable to Klippel-Feil Syndrome.
Figure 2: Imaging of this patient with Klippel-Feil Syndrome. A: Thoracic spinal column radiograph showing dextro-scoliosis without thoracic vertebral fusion. B: Sagittal T1 weighted image magnetic resonance imaging of the cervical spine showing fusion of the first three cervical vertebrae, protrusion into the cervical canal (circle), and reversal of the normal cervical curvature. C: Photograph of the patient attempting to extend her neck, demonstrating limited range of motion. Note the under-developed external ear (microtia).
Figure 3: Hypnogram data. A: Diagnostic polysomnogram. B: Bilevel positive airway pressure (BPAP) titration polysomnogram. SpO2: pulse oximetry. HR: heart rate. CA: central apneas. OA: obstructive apneas. MA: mixed apneas. HYPO: hypopneas. RERA: respiratory effort related arousals. Pos: sleep position. S: supine sleep position. L: left lateral decubitus sleep position. R: right lateral decubitus sleep position. MIC: microphone. LegMvt: leg movements. EPAP: expiratory positive airway pressure. IPAP: inspiratory positive airway pressure. During the diagnostic polsyomnogramm average pulse oximetry was 87% during non-REM and 76% during REM. During the BPAP study oxygenation improved with an average pulse oximetry of 95% during non-REM and 94% during REM.
|
Sleep Parameter |
Diagnostic Study |
Titration Study |
|
Total sleep time (minutes) |
165.5 |
271.5 |
|
Sleep Efficiency (%) |
41.9 |
84.6 |
|
% N1 |
7.6 |
0.6 |
|
% N2 |
87 |
33 |
|
% N3 |
0 |
28.7 |
|
% REM |
5.4 |
37.8 |
|
Arousal index |
39.9 |
6.9 |
|
# Obstructive apneas |
253 |
* 3 |
|
# Obstructive hypopneas |
18 |
* 8 |
|
# Central Events |
0 |
* 0 |
|
Desaturation index REM |
66.7 |
71 |
|
Desaturation Index NREM |
99.7 |
38.8 |
|
Desaturation Nadir (%) |
34 |
*92 |
Table 1: Polysomngram data. * Indicates events at final bilevel positive airway pressure (BPAP) setting of 25/21. Sleep duration at final pressure was 29.9 minutes. Mask leak was 23.4 L/min.
Question:
What is a contributory anatomic factor to this patient’s severe sleep disordered breathing?
Discussion
Klippel-Feil Syndrome is a genetically heterogenous disorder characterized by fusion of two or more cervical vertebrae. The classic triad described by Klippel and Feil of short neck, decreased cervical range of motion and low posterior hairline is found in less than 50% of patients (1). Klippel-Feil Syndrome is seen most commonly in women and has an incidence of 1:40,000 people.
Although most cases of Klippel-Feil Syndrome are sporadic, both autosomal dominant and autosomal recessive forms have been reported. Klippel-Feil Syndrome has been linked to mutations in GDF6 and GDF3 genes in some patients (2,3). The exact cause of Klippel-Feil Syndrome remains unknown.
Three morphological types of cervical vertebral fusion have been described in Klippel-Feil Syndrome (4). Type I consists of massive fusion of many cervical and thoracic vertebrae into bony blocks; Type II has fusion at only one or two interspaces; and Type III comprises both cervical fusion and lower thoracic or lumbar fusion. Our patient’s cervical vertebral fusion was consistent with Klippel-Feil Syndrome, type II, which is the most common (5).
Associated anomalies include: scoliosis, hearing loss (sensori-neural, conductive or both), ear anomalies including microtia, facial asymmetry, cleft palate, ventricular septal defects, and renal anomalies. Neurological abnormalities in Klippel-Feil Syndrome may include Arnold Chiari malformation, and cervicomedullary neuroschisis with mirror movements. (2,6). The clinical presentation varies. Younger children usually present with hearing loss, delayed milestones and mirror movements. Older patients usually present with headaches, neck pain with limited range of motion, upper extremity sensory loss, and gait disturbances. (7)
Sleep disordered breathing has been reported in patients with Klippel-Feil Syndrome (8). Its pathophysiology is multifactorial. Syndrome- specific predisposing characteristics include: the presence of hindbrain anomalies or Arnold Chiari malformation, short thick neck, decreased mobility, scoliosis and airway narrowing likely secondary to cervical vertebrae fusion with protrusion in the airway (9,10). Syndrome unrelated features that may contribute to sleep disordered breathing include: micrognathia, obesity, and upper airway anatomy.
Our patient did not have hindbrain anomalies. Figure 1 shows cervical vertebral fusion with vertebral body impingement on the posterior airway (which explains the need to use a pediatric endoscope during transnasal esophagoscopy). This airway narrowing, in combination with short neck, decreased neck extension and scoliosis are the syndrome specific factors contributing to this patient’s sleep disordered breathing. In our patient mild retrognathia and overweight are the non-syndrome related factors contributing to her severe disordered breathing.
Answer:
In addition to her short neck and scoliosis, other contributions to her severe sleep disordered breathing associated with Klippel-Feil Syndrome probably included impingement of a vertebral body bony abnormality on the posterior airway (white arrow, Figure 1).
Follow-up
The patient is compliant with positive airway pressure therapy and has noted improvement in excessive daytime sleepiness.
References
-
Tracy MR, Dormans JP, Kusumi K. Klippel-Feil syndrome: clinical features and current understanding of etiology. Clin Orthop Relat Res. 2004; (424): 183-90.
-
Tassabehji M, Fang ZM, Hilton EN, McGaughran J, Zhao Z, de Bock CE, et al. Mutations in GDF6 are associated with vertebral segmentation defects in Klippel-Feil syndrome. Hum Mutat. 2008; 29(8): 1017-27.
-
Ye M, Berry-Wynne KM, Asai-Coakwell M, Sundaresan P, Footz T, French CR, et al. Mutation of the bone morphogenetic protein GDF3 causes ocular and skeletal anomalies. Hum Mol Genet. 2010; 19(2): 287-98.
-
Gunderson CH, Greenspan RH, Glaser GH, Lubs HA. The Klippel-Feil syndrome: genetic and clinical reevaluation of cervical fusion. Medicine (Baltimore). 1967; 46(6): 491-512.
-
Woon CYL et al, Cervical spine trauma in Klippel—Feil syndrome: Two cases with contrasting outcomes and a review of the literature. Injury Extra (2007) 38, 392—396
-
Royal SA, Tubbs RS, D'Antonio MG, Rauzzino MJ, Oakes WJ. Investigations into the association between cervicomedullary neuroschisis and mirror movements in patients with Klippel-Feil syndrome. AJNR Am J Neuroradiol. 2002; 23(4): 724-9.
-
Nagib MG, Maxwell RE, Chou SN. Identification and management of high-risk patients with Klippel-Feil syndrome. J Neurosurg. 1984; 61(3): 523-30.
-
Rosen CL, Novotny EJ, D'Andrea LA, Petty EM. Klippel-Feil sequence and sleep-disordered breathing in two children. Am Rev Respir Dis. 1993; 147(1): 202-4.
-
Singh D, Mills GH, Caunt JA, Alderson JD. Anaesthetic management of labour in two patients with Klippel-Feil syndrome. Intl J of Obst Anesth. 1996; (5): 198-201.
-
Lee JJ, Lim BG, Lee MK, Kong MH, Kim KJ, Lee JY. Fiberoptic intubation through a laryngeal mask airway as a management of difficult airwary due to the fusion of the entire cervical spine - A report of two cases. Korean J Anesthesiol. 2012; 62(3): 272-6.