Contributed by Contributed by Lourdes DelRosso, MD, Justin Liegmann, M.D Division of Sleep Medicine, Department of Neurology Louisiana State University Health Sciences Center, Shreveport LA Corresponding Author Lourdes DelRosso, MD Assistant Professor Sleep Medicine Division of Sleep Medicine, Department of Neurology Louisiana State University School of Medicine
In Brief
A sleep medicine physician observed unusual patient movements recorded during an overnight in-laboratory CPAP titration study. The observed movements generated a differential diagnosis that was considered in the context of other information revealed in the patient’s medical history and her polysomnogram.
A 33-year-old woman presented for further evaluation of sleep-onset insomnia, snoring, and excessive daytime sleepiness. Among other chronic medical problems, she had hypertension, was morbidly obese and suffered from post-traumatic neuropathic pain involving the lower extremities. There was no history of traumatic brain injury or seizures. She initially denied any history of sleepwalking or other potentially injurious behavior during sleep. However she typically sleeps alone, so abnormal behavior during sleep went largely unwitnessed. Medications included paroxetine, amlodipine, cyclobenzaprine, lisinopril, metformin, metoprolol, gemfibrozil, omeprazole, pravastatin, topiramate, trazodone, and tramadol. She denied alcohol use.
Physical examination revealed an obese woman with a body mass index (BMI) of 47 kg/m2. Epworth sleepiness score was 8/24. Her neck circumference was 18 inches (47 cm). The posterior airway was crowded (Mallampati IV) with a large tongue showing lateral scalloping on protrusion.
Polysomnographic testing was performed, which revealed obstructive sleep apnea (OSA) with an apnea hypopnea index of 5 per hour of sleep. The minimum oxygen saturation was 88%. The patient was supine for 94% of the recording. Sleep Efficiency was 92%. All stages of sleep were noted, with REM sleep comprising 13% of the total sleep time (TST). No unusual behaviors were noted during this study.
The patient returned for a full night in-laboratory continuous positive airway pressure titration study. During this study, the interpreting sleep physician noted unusual movements occurring spontaneously during rapid eye movement (REM) sleep (see Video 1 and figures 1 and 2). Aside from the series of movements shown in the video, no other unusual behavior was noted. REM comprised 11% of the TST and Sleep Efficiency was 97%.
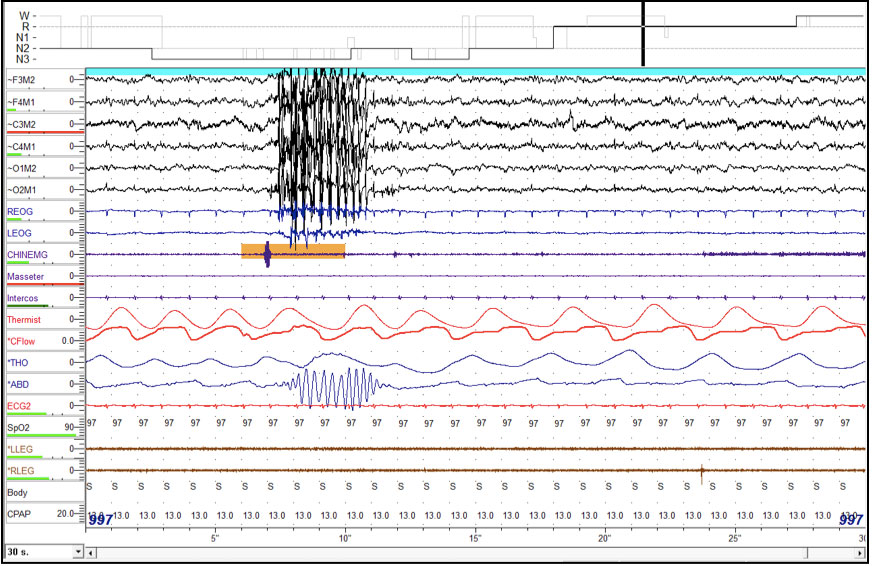
Figure 1: 30-second epoch during REM sleep showing repetitive movements with a frequency of 3 Hz.
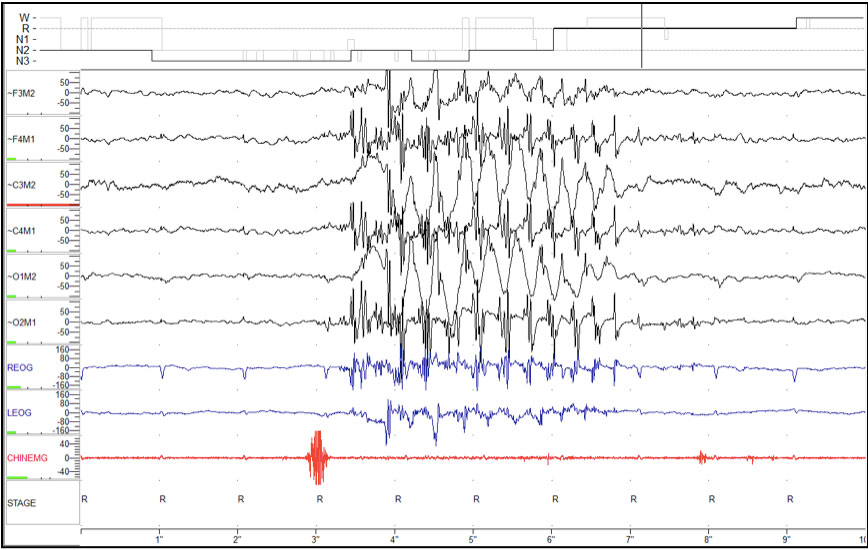
Figure 2: 10-second epoch during REM sleep, demonstrates movement artifact on EEG channels with a frequency of 3 Hz.
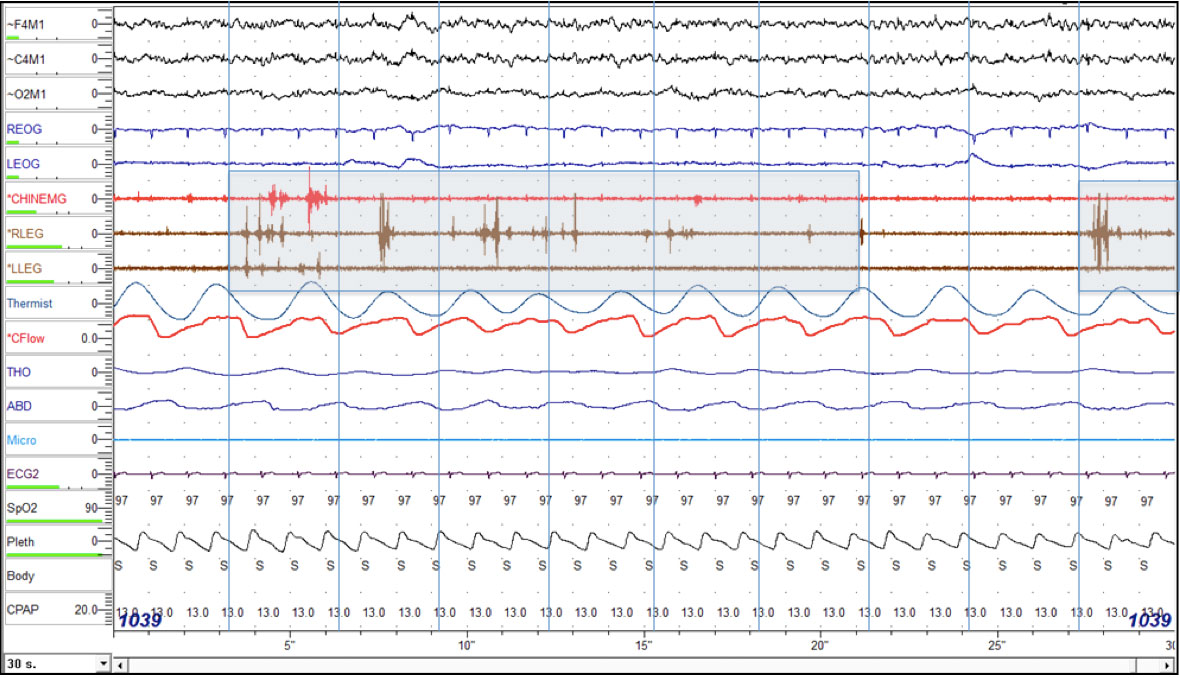
Figure 3: 30-second epoch during REM fulfills criteria for phasic REM sleep without atonia. The vertical blue lines divide the epoch into ten 3-second mini epochs. Increased transient muscle activity in the leg and chin leads is seen in the shaded mini epochs (rule F-1) (3)
Question:
What is the best way to characterize the movement episode shown in video 1?
Discussion
The differential diagnosis for abnormal behaviors during sleep includes sleep-related seizures, rhythmic movement disorders of sleep (RMDS), NREM arousal parasomnias (e.g. sleepwalking, confusional arousals, night terrors), and REM parasomnias (e.g. REM sleep behavior disorder [RBD]).
Seizures that occur during sleep may mimic parasomnias. The fact that this patient had no past history of seizures makes this option less likely, but does not rule it out; some patients have seizure activity exclusively during sleep. The sleep-related polysomnogram montage is insensitive for excluding a diagnosis of sleep related seizures. However, the absence of abnormal wave morphology on the EEG (spike and wave, polyspikes), the presence of the event during REM sleep (which is typically the least-likely sleep stage in which seizures will occur), the lack of an autonomic response to the event (the heart rate was stable) and the absence of post-event generalized slowing of EEG waveform all make seizure a less credible explanation.
The international classification of sleep disorders, second edition, defines RMDS as repetitive, stereotyped and rhythmic motor behaviors that involve large muscle groups; occur during periods of drowsiness; result in a significant complaint (bodily injury, interference with sleep or daytime impairment); are not better explained by another current sleep, medical, mental or neurological disorder; and are not associated with medication or substance use.(1) This group of disorders includes head rolling, body rocking, and head banging.
Commonly encountered during infancy, RMDS have been shown to persist into adulthood in a small percentage of patients, sometimes in association with genetic factors or psychiatric comorbidities (depression, obsessive compulsive behavior and attention deficit hyperactivity disorder).(2) The criteria for scoring RMDS during a polysomnogram include: Minimum frequency of 0.5 Hz, maximum frequency of 2 Hz, 4 minimum number of individual movements, and an amplitude of 2 times the background EMG activity.(3) RMDS have been reported during both NREM and REM sleep, however cases during REM sleep are not typically associated with REM sleep without atonia (RSWA).(4) The co-existence of RBD and RMDS has also been reported, with RMDS seen during both NREM and REM sleep.(5)
While this patient’s behavior appears at first glance to be consistent with RMDS arising from REM sleep, further inspection reveals that the frequency of her movements (3 Hz) was faster than that typically described with RMDS (Figures 1 and 2). Additionally review of this patient’s other epochs of REM revealed the presence of frequent RSWA, both during her diagnostic polysomnogram and during the positive airway pressure (PAP) titration study (Figure 3)
Confusional arousals typically create behaviors that appear willful though heavily impaired, similar to intoxication. Movements are often slow and uncoordinated. Confusional arousals selectively occurring from REM sleep may occur in patients with OSA, due to worsening REM-related respiratory status. The behavior noted in this video would be an unusual pattern to be seen during a confusional arousal. In addition, the absence of characteristic electroencephalogram (EEG) patterns of wakefulness precludes the diagnosis of confusional arousal.
Our patient’s episode fulfills the American Academy of Sleep Medicine criteria for RBD by virtue of excessive REM sleep without atonia, abnormal REM behavior documented during PSG and absence of epileptiform activity on EEG.(1) Serotonergic medications such as paroxetine have been associated with REM sleep without atonia, REM behavior disorder, and Periodic Leg Movements of Sleep.(6, 7) Given this patient’s ongoing therapy with a selective serotonin reuptake inhibitor (SSRI), RBD secondary to medication use is a strong possibility.
This patient’s history was reviewed in detail, and she revealed that in the past she had been informed that she occasionally appears to cry out or move purposefully about in bed, with behaviors appearing to an onlooker as if acting out in her dreams. Because these events neither caused social problems nor any personal injury, she had never brought them to the attention of a physician.
Answer
The video is most compatible with REM sleep behavior disorder, presenting as a pseudo-rhythmic movement disorder.
Follow-Up
Three months later, she was found to be compliant with PAP therapy, with a resolution of sleep-related complaints and a reduction in daytime sleepiness. She specifically denied any problems resulting from dream enactment behavior. The option of switching her SSRI to an agent less likely to provoke RBD (e.g.: bupropion) was discussed with the patient as a future possibility, should dream enactment behavior become a cause for clinical concern. She decided to continue on her current medications for now.
References
-
American Academy of Sleep Medicine. International classification of sleep disorders; diagnostic and coding manual. 2nd edition. ed. Westchester, IL: American Academy of Sleep Medicine; 2005.
-
Stepanova I, Nevsimalova S, Hanusova J. Rhythmic movement disorder in sleep persisting into childhood and adulthood. Sleep. 2005 Jul;28(7):851-7.
-
Iber C, American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events : rules, terminology, and technical specifications. Westchester, IL: American Academy of Sleep Medicine; 2007.
-
Kempenaers C, Bouillon E, Mendlewicz J. A rhythmic movement disorder in REM sleep: a case report. Sleep. 1994 Apr;17(3):274-9.
-
Winkelman JW, James L. Serotonergic antidepressants are associated with REM sleep without atonia. Sleep. 2004 Mar 15;27(2):317-21.
-
Hoque R, Chesson AL, Jr. Pharmacologically induced/exacerbated restless legs syndrome, periodic limb movements of sleep, and REM behavior disorder/REM sleep without atonia: literature review, qualitative scoring, and comparative analysis. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2010 Feb 15;6(1):79-83.