Unwanted Residents in the Pleural Space:
Polymicrobial Growth in Empyema as an Indicator for Esophageal Pleural Fistula
Fahid Alghanim, MD, Pulmonary and Critical Care Fellow, Department of Internal Medicine, Division of Pulmonary and Critical Care, University of Maryland School of Medicine
Ellen Marciniak, MD, Assistant Professor, Department of Internal Medicine, Division of Pulmonary and Critical Care, University of Maryland School of Medicine
Case:
A 59-year-old man with a history of COPD and unresectable stage IIIA Squamous Cell Carcinoma of his Right lower Lobe (RLL) in 2012 treated with concurrent chemo- and radiation therapy who had pathologically proven local recurrence of disease in 2018 which was treated with combined chemotherapy (Carboplatin & Abraxane) and Immune Modulate Proton Therapy (IMPT) (6120 cGy) presented with 2 weeks of progressively worsening dyspnea and pleuritic chest pain.
On evaluation, he was tachycardic with fever (38.6 °C) and exhibited decreased air entry to his RLL. Contrast enhanced Computed Tomography (CT) of the chest was done and showed right middle and lower lobe consolidation with areas of cavitation and a moderate right sided pleural effusion (Image 1). The patient was started on broad spectrum antibiotics. A repeat CT chest was obtained on day 7 due to clinical deterioration, which showed a new right-sided hydropneumothorax (Image 2). A pigtail chest tube was placed by Interventional Radiology that drained brown, markedly turbid fluid that was exudative based on Light’s criteria (pH < 6.3, LDH 575). His chest tube output continued to drain copious volume (average: 400 ml/day) of turbid, foul-smelling fluid with particulate matter over the next few days. Microbiological data identified polymicrobial growth of oral/upper respiratory tract: GPC in pairs and chains, GPRs, and candida glabrata. Subsequent CT chest after chest tube placement is shown below (Image 3):
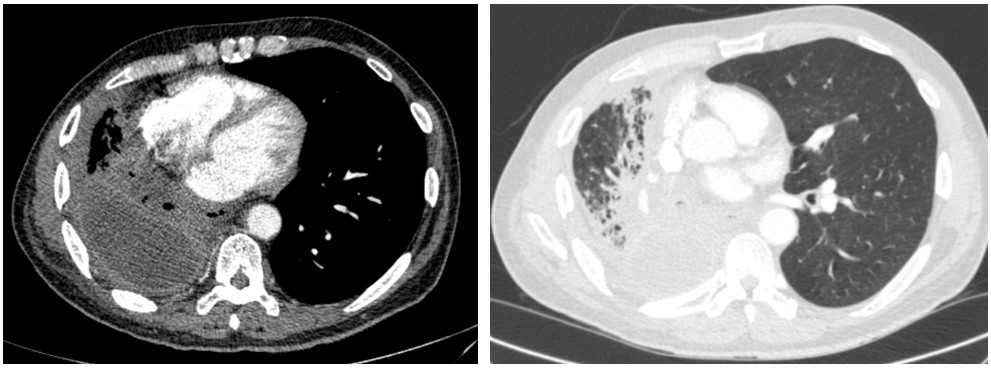
Image 1 demonstrates right middle and lower lobe consolidation with areas of cavitation and a moderate right sided pleural effusion.
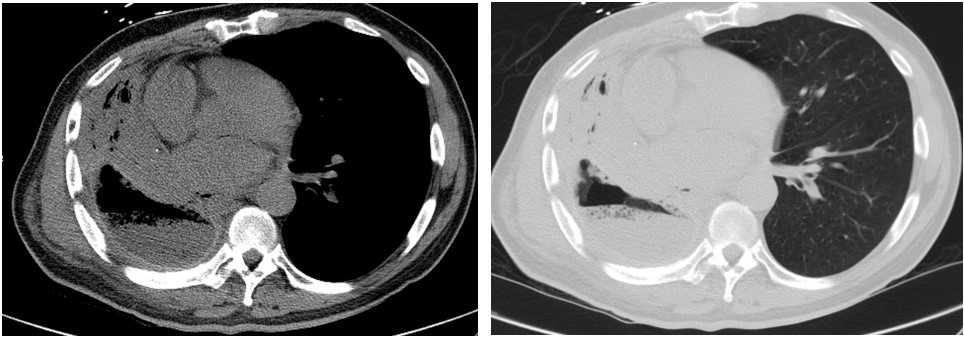
Image 2 demonstrates the development of a new hydropneumothorax.
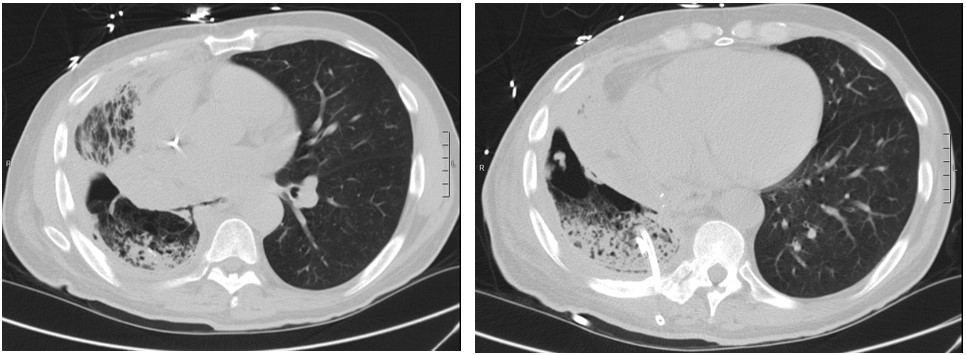
Image 3 is shown above.
Question:
What is the most likely cause of his clinical symptoms?
- Bronchopleural Fistula
- Esophageal pleural fistula
- Lung Abscess
- Iatrogenic Hydropneumothorax
B. Esophageal pleural fistula
Discussion:
The CT chest associated with image 3 demonstrates a fistulous connection between the lower esophagus and the right pleural space, which is diagnostic of an esophageal pleural fistula (EPF). EPF continues to be a rare clinical entity that is very difficult to identify. It is reported to occur most often as a result of an insult to the esophageal vascular supply in the setting of pneumonectomy (1). The esophagus is in direct contact with the right pleural space for a considerable distance as compared to the left pleural space which is mostly shielded by the anatomical position of the descending aorta. Therefore, right sided EPF are more frequently encountered, as was demonstrated in our patient (2). Salient features of EPF are pleural drainage correlating with oral intake, polymicrobial growth on culture data, and evidence of hydropneumothorax on chest imaging in a host that is at risk (1-5). These risk factors include intrathoracic malignancy, radiation therapy, thoracic instrumentation, and esophageal inflammation (2). Initially, patients with EPF will need to be made NPO and should be given broad spectrum intravenous antimicrobials, which may include antifungal agents (6). When this patient was made NPO, his chest tube drainage dropped acutely to zero. More definitive treatment includes reconstruction of the esophageal wall with the assistance of colleagues from gastroenterology and cardiothoracic surgery followed by obliteration of the empyema cavity.
This patient underwent endoscopic stenting and suturing of his esophageal wall by gastroenterology.
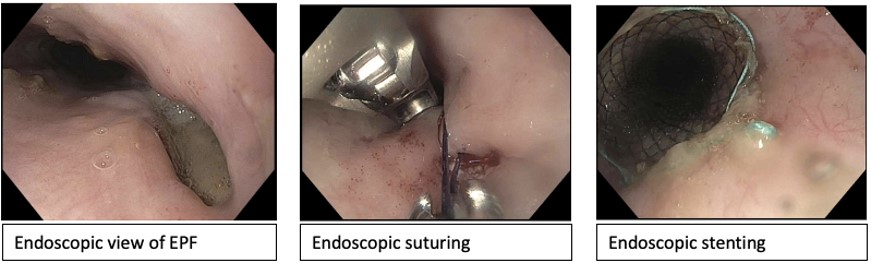
Thereafter, he was transitioned from total parenteral nutrition to oral feeds after confirmation of closure of his fistula by esophagram and was discharged home in a stable condition. Unfortunately, his course was further complicated by recurrence of his fistula and he required multiple interventions by cardiothoracic surgery including esophageal vacuum therapy as well as multiple esophageal flaps over an extended period of time. Although IMPT provides the advantage of delivering higher doses of radiation to cancer cells and lower to normal tissues, in this particular patient it may have been an important contributing factor to the development of EPF as well as further complications and failures of therapeutic interventions.
Answer choice A) Although bronchopleural fistula (BPF) is in the differential diagnosis of hydropneumothorax, it is unlikely in our case given the lack of connection between bronchus and pleural space on imaging. Moreover, a BPF would cause a persistent air leak not persistent pleural fluid drainage. Answer choice C) lung abscess would show an abnormality within the lung parenchyma rather than the pleural space as in this case. Answer choice D) Iatrogenic hydropneumothorax was present before the chest tube was placed and is not the underlying etiology of this patient’s presentation.
References
-
Simultaneous bronchopleural and esophagopleural fistulas after pneumonectomy. Trigui W., Le Pimpec-Barthes F., Shaker W., Lang-Lazdunski L., Riquet M.(2002) Annals of Thoracic Surgery, 74 (3) , pp. 923-924.
-
Sachdeva R, Sachdeva S. Esophageo pleural fistula due to esophageal cancer. J Assoc Chest Physicians 2015;3:23-4
-
Eguchi, K., Ogura, M., Hisaoka, K. et al.Successful treatment of esophagopleural fistula following pulmonary resection for primary lung cancer: a case report. surg case rep 5, 78 (2019) doi:10.1186/s40792-019-0638-1
-
Kumar S, Singh A, Matreja PS, Kler SK. A case report of a spontaneous oesophageal pleural fistula. J Clin Diagn Res. 2013;7(3):522–524. doi:10.7860/JCDR/2013/4950.2811
-
Desai, P., Asharaf, A., Wang, Y., Mathew, M., Jaiswal, P., Mutneja, H., & Alebich, M. (2018). A Strange Connection: Spontaneous Esophageal-Pleural Fistula. American Journal of Gastroenterology, 113(Supplement). doi: 10.14309/00000434-201810001-01750
-
Al-Shawwa B, D'Andrea L, Quintero D. Candida esophageal perforation and esophagopleural fistula: a case report. J Med Case Rep. 2008;2:209. Published 2008 Jun 17. doi:10.1186/1752-1947-2-209



