Real Time Therapeutic Thoracentesis
Gupta, Preeti MD MPH 1; Yamanaka, Travis MD 1 ,2; Kovitz, Kevin MD 1, 3
1 University of Illinois Chicago, Division of Pulmonary, Critical Care, Sleep and Allergy, Chicago IL
2 Jesse Brown Veterans Affairs Medical Center, Chicago IL
3 Chicago Chest Center, Elk Grove, IL
Case
A 79-year-old male with a past medical history of Alzheimer’s dementia, chronic respiratory failure with tracheostomy and ventilator dependence, end stage renal disease, and atrial fibrillation is admitted to the intensive care unit from an outside hospital with septic shock. Urine cultures were positive for Vancomycin-resistant Enterococcus faecium and the tracheal aspirate was positive for Stenotrophomonas, Pseudomonas, and Proteus species. Chest x-ray demonstrated a right pleural effusion, which was present since outside hospital admission two and a half weeks prior. Decision was made to drainto rule out a source of persistent septic shock. Ultrasound guided thoracentesis was performed with ultrasound visualization during therapeutic aspiration. A total of 1400 cc of serous fluid was removed. After the procedure, the patient was briefly hypotensive, which resolved without intervention. Oxygenation remained stable. Pleural studies revealed a paucicellular lymphocytic transudate.
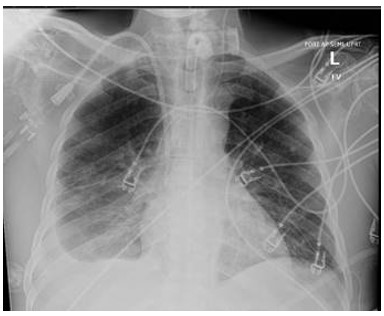
Figure 1: Chest X-ray obtained prior to thoracentesis demonstrating free flowing pleural effusion on the right.
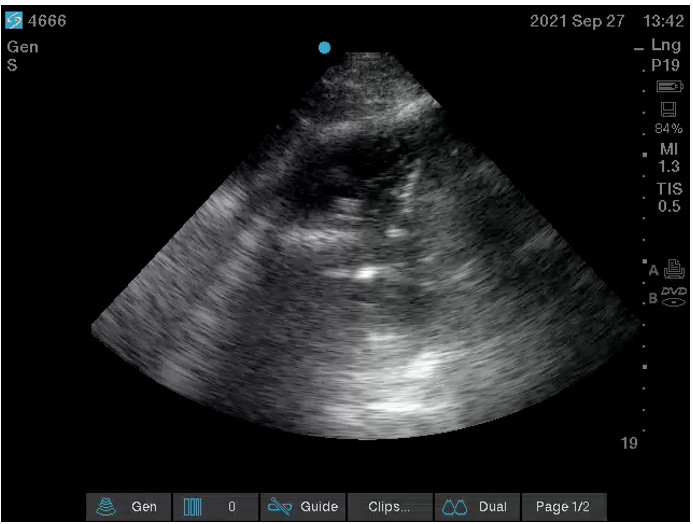
Figure 2: Ultrasound video clip obtained during therapeutic aspiration of pleural fluid

Figure 3: Upright Chest X-ray performed post procedure
Question
What is the finding?
- Tension pneumothorax
- Pneumothorax ex vacuo
- Re-expansion pulmonary edema
- Hemothorax
What is the immediate next step?
- Emergent needle decompression
- Observation
- Diuresis
- Insert a large bore chest tube (28 to 32 French)
B. Pneumothorax ex vacuo
B. Observation
Discussion
The ultrasound image revealing air bubbles in the effusion after partial drainage and the post-procedure upright chest x-ray demonstrating a basilar pneumothorax without a substantial change in the volume of pleural space suggest pneumothorax ex vacuo (1). Tension pneumothorax due to iatrogenic lung injury is incorrect because the patient’s hypotension was transient and resolved without intervention. In addition, there is no mediastinal shift on chest radiograph. The Chest x-ray does not demonstrate cephalization of lung vasculature, peri-bronchial cuffing, or septal lines to suggest pulmonary edema. There is no pleural opacification or blunting of the costophrenic angle to suggest hemothorax.
Pneumothorax ex vacuo can be a clinical presentation of trapped or entrapped lung (2). Management of unexpandable lung depends on the underlying process. If the pleural process is still active, such as in empyema or complex parapneumonic effusion, pleural malignancy, post-cardiac surgery, rheumatoid pleuritis, or uremic pleuritis; it is termed lung entrapment. Treating the underlying inflammatory process can help improve lung entrapment. In trapped lung, the inflammatory pleural process has resolved leaving behind a fibrous peel, resulting in a more permanent condition (2). In this case, if the patient is asymptomatic and radiologic appearance is stable, additional diagnostic or therapeutic interventions are not acutely indicated. Thus, the appropriate next step in management would be observation. In symptomatic patients with extensively trapped lung, surgical decortication is considered.
Unexpandable lung is characterized by a lack of apposition of the parietal and visceral pleura after therapeutic drainage. Excessive negative intrapleural pressures during drainage can result in a transient pressure-dependent fistula between the pleural space and the lung parenchyma or the environment, which aims to equilibrate intra and extra-pleural pressures. This excessive negative pressure during drainage occurs either because of mechanical restriction of lung expansion by a visceral pleural thickening or bronchial obstruction.
Pneumothorax ex vacuo occurs only after large volume therapeutic thoracenteses and not with diagnostic or low-volume thoracenteses. Pleural manometry during the procedure has not been shown to prevent this finding (1). Heidecker and colleagues postulated that this may be due to regional variability in pleural elastance resulting in non-uniform measurement. Another multicenter study reproduced this finding (3). The authors suggested that this may be due to non-continuous measurements that do not detect acute pressure changes and may create a false sense of reassurance leading to a greater volume of fluid drainage.
References
-
Heidecker J, Huggins JT, Sahn SA, Doelken P. (2006) Pathophysiology of pneumothorax following ultrasound-guided thoracentesis. Chest, 130 (4): 1173-1184
-
Huggins, J.T., Maldonado, F., Chopra, A., Rahman, N. and Light, R. (2017) Unexpandable lung from pleural disease. Respirology, 23: 160– 167
-
Lentz RJ, Lerner AD, Pannu JK, Merrick CM, Roller L, Walston C, Valenti S, Goddard T, Chen H, Huggins JT, Rickman OB, Yarmus L, Psallidas I, Rahman NM, Light RW, Maldonado F (2019) Routine monitoring with pleural manometry during therapeutic large-volume thoracentesis to prevent pleural-pressure-related complications: a multicentre, single-blind randomised controlled trial. Lancet Respir Med, 7(5):447-455.



