Lung Protective Ventilation: More Than Simply Setting the Tidal Volume
Souvik Chatterjee, MD
Department of Critical Care Medicine, Department of Pulmonary Medicine.
Medstar Washington Hospital Center.
Case
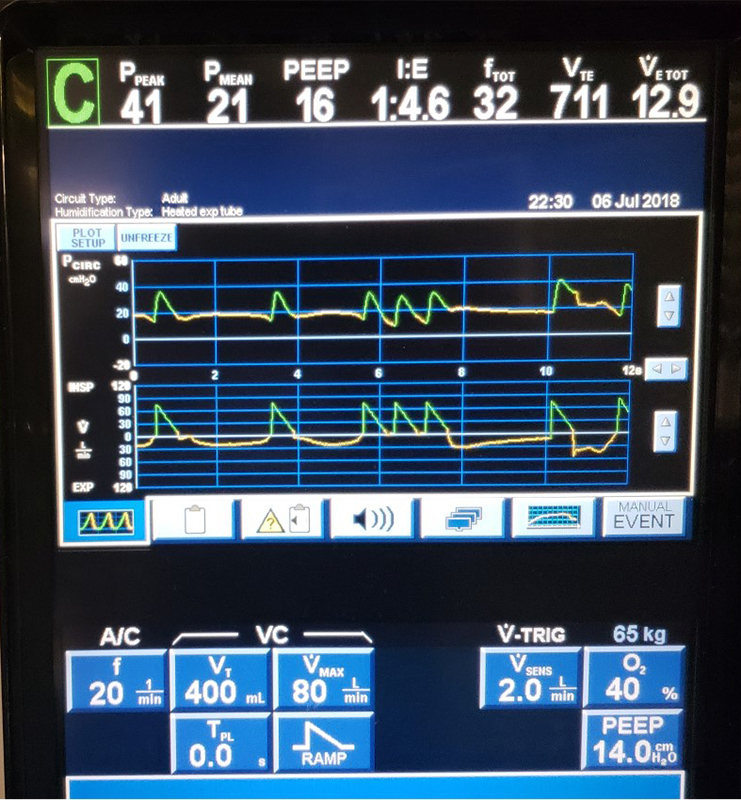
A 65-year-old female with a history of peripheral arterial disease (PAD), coronary artery disease (CAD), and s/p CABG 5 years ago presented with acute right sided weakness and was found to have an ischemic stroke in the MCA distribution. She was intubated for mechanical thrombectomy after tPA administration and persistent symptoms. Post-procedure, she was profoundly hypoxic with 02 saturation of 88% on FiO2 1.0 and PEEP 14 cm H20. A lung protective ventilation strategy was initiated using Volume Assist Control ventilation with TV of 6 cc/kg of IBW, PEEP was up-titrated and inhaled epoprostenol was initiated. The patient was sedated with dexmedatomidine and PRN fentanyl. Representative ventilator waveforms are shown below.
Question
The waveforms reveal what potential ventilator associated lung injury risk?
- Delayed Cycling
- Atelectrauma
- Auto-triggering
- Barotrauma
Answer: D. Barotrauma
Discussion
This patient was diagnosed with moderate ARDS based on the acute onset of bilateral infiltrates and respiratory failure not completely explained by cardiac failure and fluid overload.1 In order to minimize ventilator associated lung injury (VALI), specifically macro and micro barotrauma, a low tidal volume strategy of 6 cc/kg of IBW was instituted based on the landmark ARDSNet study.2 Additionally, with the goals to minimize delirium and promote early mobility, sedation was intentionally minimized.3
The waveform image demonstrates both cycling and triggering asynchronies, premature cycling and ineffective triggering, respectively. A premature cycle results when the patient’s neural inspiratory time is prolonged relative to the ventilator’s set inspiratory time. Premature cycling can be identified on the first two breaths of the flow waveform, where at the beginning of expiration there is a notch or delay in expiratory flow (less expiratory flow then expected) indicating a continuation of the patient’s inspiratory effort beyond the ventilator’s preset inspiratory time (red arrow). This problem results in excessive work of breathing and likely elevated transpulmonary pressures for the patient as they continue to inspire against a closed ventilator inspiratory valve. During expiration the expiratory flow curve has a flattened appearance indicating active exhalation until the next inspiration begins, which also adds to the patient’s work of breathing.
The 3rd through 5th breaths (red circle) demonstrate what is colloquially known as “breath stacking” but more accurately can be described as a severe premature cycling. The patient’s prolonged inspiratory effort relative to the machine’s set inspiratory time repeatedly triggers the ventilator, resulting in consecutive delivery of the preset Vt. In this case, the patient receives the prescribed 400 cc (6cc/kg IBW), three times sequentially resulting in an inhaled tidal volume of 1200cc or 18cc/kg IBW. A tidal volume of 1.2 L poses significant risk of barotrauma and volutrauma and is in direct opposition with the consensus recommendations for ARDS.4 Additionally, on the final breath of the scalar, there is a trigger asynchrony, specifically an ineffective trigger (yellow arrow), that is most likely due to an increase in end-expiratory volume and pressure following the delivery of three successive mandatory-volume breaths. Triggering and cycling asynchronies increase the patient’s work of breathing and increase the risk of barotrauma.5,6
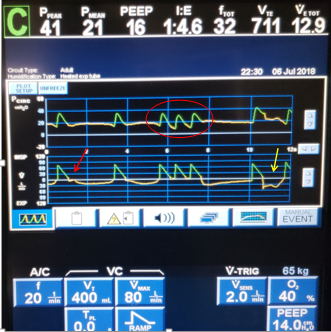
For these reasons, the ventilator’s inspiratory time was increased (by decreasing the peak inspiratory flow rate and increasing the tidal volume to 8cc/kg IBW). However, these adjustments alone failed to resolve the premature cycling, so the patient was also started on a continuous propofol infusion and was paralyzed with intermittent vecuronium, resulting in improvement in PaO2 by 50 mm Hg. The PEEP was subsequently titrated down, and the patient was liberated from mechanical ventilation within 48 hours.
References:
-
The ARDS Definition Task Force. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012; 307(23): 2526–33.
-
The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes compared with traditional volumes for acute lung injury and acute respiratory distress syndrome. NEJM 2000; 342: 1301-8.
-
Vasilevskis E, Ely E, Speroff T, et al. Reducing iatrogenic risks: ICU-acquired delirium and weakness-crossing the quality chasm. Chest 2010; 138(5): 1224-33.
-
Fan E, Del Sorbo L, Goligher E, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 2017; 195(9): 1253-63.
-
Epstein S. How often does patient-ventilator asynchrony occur and what are the consequences. Respir Care 2011; 56(1): 25–35.
-
Mauri T, Cambiaghi B, Spinelli E, et al. Spontaneous breathing: a double-edged sword to handle with care. Ann Transl Med 2017; 5(14): 292.



