Houston, We Have a Problem
Authors: Shilpa Pandey M.D1,4., Rohini Coorg M.D.2,4, Sherrill Mohan, BS RPSGT1, Kevin Kaplan, M.D.1,3,4
- Texas Children’s Hospital Sleep Center. Houston Texas USA
- Texas Children’s Hospital. Pediatric Neurology. Houston Texas USA
- Texas Children’s Hospital. Pediatric Pulmonary. Houston Texas USA
- Baylor College of Medicine. Houston Texas USA
Case
An 18-year-old male with cerebral palsy, global developmental delay, spastic quadriplegia, and static encephalopathy secondary to hypoxic ischemic injury in the perinatal period presents with excessive sleepiness during therapy sessions. His blood gas was PH 7.39/PC02-49/P02-53/ HCO3-33 with history of poor airway clearance, recurrent pneumonias and aspiration to thin liquids on swallow study. He was evaluated using a baseline PSG and subsequent PAP titration. Current medications include baclofen 40 mg three times daily, clonazepam 0.5 mg daily, clonidine 0.1 mg at bedtime.
An MRI of the brain shows diffuse encephalomalacia involving the supratentorial brain parenchyma with volume loss of the cerebellum, the pons, and brain stem. (Figure 1)
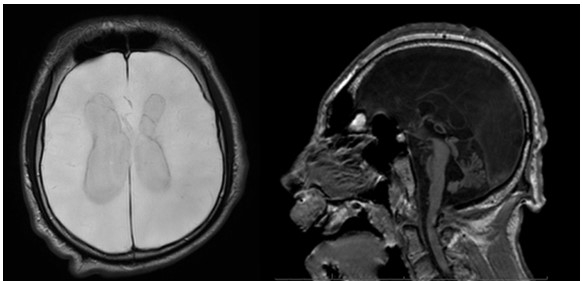 Figure 1: Axial (T2 flair) and Sagittal (T1) MRI images
Figure 1: Axial (T2 flair) and Sagittal (T1) MRI images
The diagnostic baseline polysomnogram showed moderate obstructive sleep apnea (oAHI 9.73) and central sleep apnea (cAHI 5.84) without significant hypoxemia (SpO2 nadir 90%), or hypercapnia (TcCO2 max 48 mmHg).
He returned for a PAP titration study where he was titrated to BiPAP ST 8/4 cm H20 with rate of 10 bpm. Since then, while awake, he shows no evidence of hypoxemia or hypercapnia on room air and HCO3 has improved to 26.
The baseline polysomnogram study was scored as REM/NREM as specific sleep architecture was not identified on EEG. During the polysomnogram his EEG was noted to be abnormal (Figures 2 & 3).
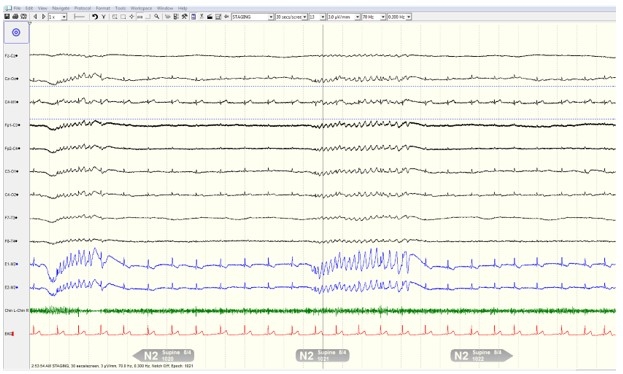 Figure 2: 30 Second Epoch During NREM Sleep
Figure 2: 30 Second Epoch During NREM Sleep
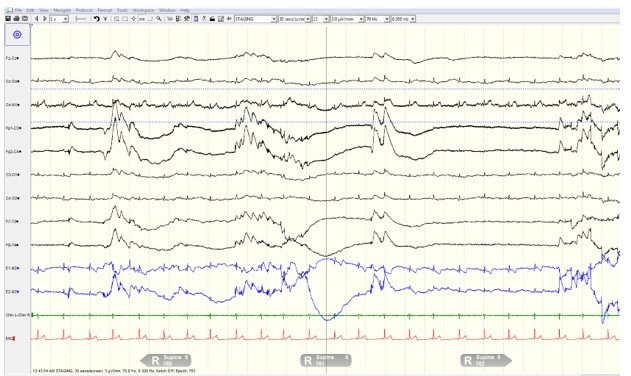 Figure 3: 30 Second Epoch During REM Sleep
Figure 3: 30 Second Epoch During REM Sleep
Question
What is the finding associated with the EEG?
- Equipment failure
- Burst suppression of the EEG
- Decrement associated with seizure activity
- Loss of signal due to hydrocephalus
- Sedation from medications
B) Burst suppression of the EEG
Discussion
Burst suppression is a finding on electroencephalography (EEG) associated with severe encephalopathy associated with coma, severe infantile-onset epilepsy syndromes, or hypothermia. It can also be medically induced by general anesthesia and is a characteristic phenomenon of deep anesthesia. It presents as a pattern of alternating high-voltage (75-250µV) activity separated by periods of suppressed voltages (less than 5µV) of electrical brain activity1. The duration of the high voltage activity is 1-20 seconds while the suppression lasts longer than 10 seconds1. When not medically induced, burst suppression is a known marker of poor prognosis.
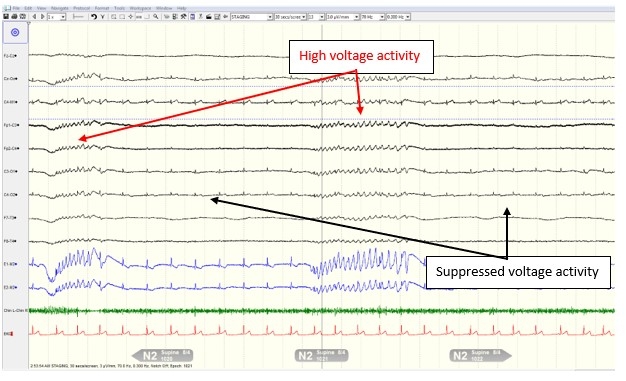 Figure 2: 30 Second Epoch During NREM Sleep with EEG changes identified
Figure 2: 30 Second Epoch During NREM Sleep with EEG changes identified
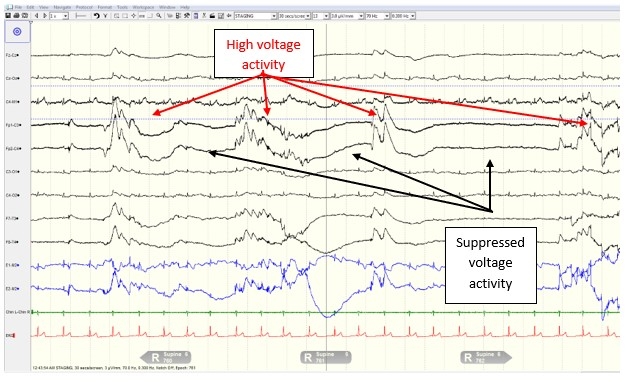 Figure 3: 30 Second Epoch During REM Sleep with EEG changes identified
Figure 3: 30 Second Epoch During REM Sleep with EEG changes identified
An MRI of the brain shows diffuse encephalomalacia involving the supratentorial brain parenchyma with volume loss of the cerebellum, the pons, and brain stem. Despite our patient’s significant underlying neurological abnormality, he can maintain adequate ventilation and oxygenation while awake. While asleep, he has moderate obstructive and central sleep apnea without hypoxemia or hypercapnia. This is likely due to the sparing of the respiratory control centers despite significant volume loss noted on the brain.
Answer A is incorrect, although evaluation of equipment failure, such as a faulty headbox, is important, the EEG demonstrates a waxing and waning of the signals. We would expect persistent loss of signal in equipment failure.
Answer C is incorrect as spike and waves consistent with seizures were not observed. The EEG is abnormal; however, seizure activity was not present during the polysomnogram.
Answer D is incorrect even though the ventricles are enlarged on brain MRI. Severe hydrocephalus can result in loss of EEG signal if there is significant buildup of fluid between the brain and skull resulting in poor signal transduction. This would result in a dampening of signals throughout the study.
Answer E is incorrect, although sedation from medication can cause burst suppression, the level of sedation required is general anesthesia. Effects from antiepileptics or sleep aids will not produce the level of sedation required to produce burst suppression.
References
-
Bhattacharyya S, Biswas A, Mukherjee J, et al. Detection of artifacts from high energy bursts in neonatal EEG. Comput Biol Med. 2013;43(11):1804-1814. doi:10.1016/j.compbiomed.2013.07.031
-
Lee J, Song WJ, Lee HW, Shin HC. Novel Burst Suppression Segmentation in the Joint Time-Frequency Domain for EEG in Treatment of Status Epilepticus. Comput Math Methods Med. 2016;2016:2684731. doi:10.1155/2016/2684731



