Holes in the Chest
Shishir Rao, DO; Internal Medicine Resident, University of Arizona. Department of Medicine.
Swathy Puthalapattu, MD; Clinical Assistant Professor, University of Arizona. Division of Pulmonary and Critical Care Medicine.
Case:
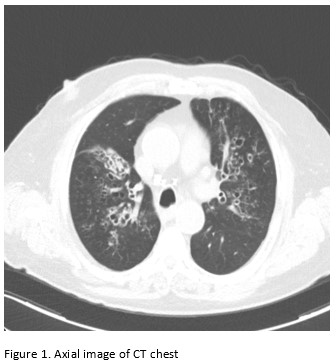
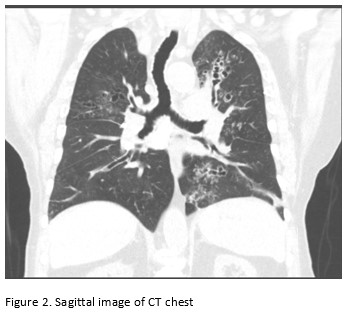
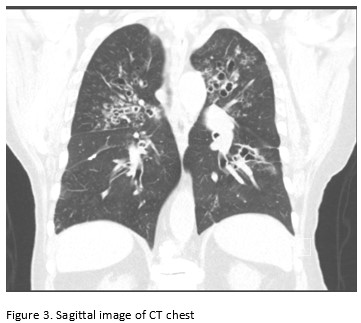
A 65-year-old male with poor healthcare follow-up presents to the pulmonary clinic with “years of breathing problems”. He reports shortness of breath and cough productive of grayish-brown sputum. He denies fevers, chills, weight loss, hemoptysis and night sweats. He denies recent travel history. His physical exam is significant for scattered wheezes bilaterally. Labs are significant for peripheral eosinophilia of cells/microL (21.7% eosinophils) and elevated total Ig E level of 2385 IU/ml. Representative images of his CT chest are shown below.
Images:
Question:
What is the most likely diagnosis?
- Eosinophilic granulomatosis with polyangiitis
- Loeffler’s pneumonia
- Allergic bronchopulmonary aspergillosis
- Alpha 1 antitrypsin deficiency
C. Allergic bronchopulmonary aspergillosis
Discussion:
Central bronchiectasis is a frequent feature of allergic bronchopulmonary aspergillosis (ABPA) and affects airways in the central one-half to two-thirds of the chest. Upper and middle lobes are most commonly affected. Although central bronchiectasis is often associated with ABPA, it is neither sensitive nor specific. Other causes of bronchiectasis with central predominance include congenital tracheobronchomegaly (Mounier Kuhn syndrome) and Williams Campbell syndrome 1.
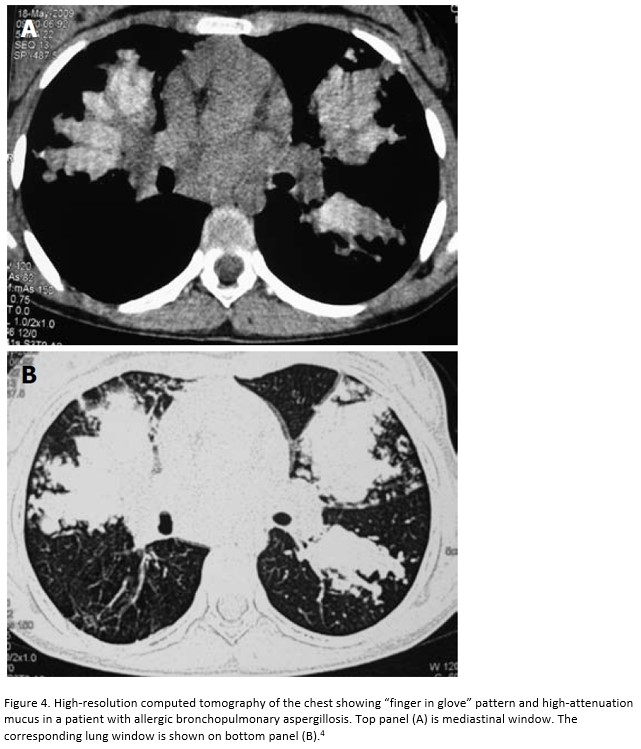
ABPA is an immunologically mediated disease with hypersensitivity against the antigens of Aspergillus fumigatus2. Diagnosis of ABPA is established in patients with asthma and cystic fibrosis with a total serum Ig E level >1000 IU/ml and presence of aspergillus skin test positivity and Ig E levels against Aspergillus fumigatus. Peripheral eosinophilia can also be seen with levels typically > 500 cells/microL. However, many patients can present with levels <500 cells/microL (as seen in this patient)3. The “finger in ” sign can be seen on radiographic imaging due to intrabronchial exudates and bronchial wall thickening. High attenuation mucus, defined as mucus radiographically denser than skeletal muscle is seen in 18- 28% of cases. High-attenuating mucus represents fungal debris containing iron and (Figure 4).
Our patient was diagnosed with asthma and ABPA. His pulmonary function test showed moderate to severe obstructive defect with significant bronchodilator response. He was initially treated with prednisone 40 mg by mouth. Few months later, due to ineffective control of symptoms, itraconazole 200 mg po daily was added. Due to slow resolution of symptoms and persistently elevated IG E level, both medications were continued for a period of 2.5 years before stopping them. Patient is currently stable on budesonide/formoterol and albuterol inhalers and is being followed in pulmonary clinic once a year.
References
-
Milliron B1, Henry TS1, Veeraraghavan S1, Little BP. Bronchiectasis: Mechanisms and Imaging Clues of Associated Common and Uncommon Diseases. 2015 Jul-Aug;35(4):1011-30.
-
Rosenberg M, Patterson R, Mintzer R, Cooper BJ, Roberts M, Harris KE: Clinical and immunologic criteria for the diagnosis of allergic bronchopulmonary aspergillosis. Ann Intern Med. 1977, 86:405-414.
-
Shah A, Panjabi C: Allergic bronchopulmonary aspergillosis: a perplexing clinical entity. Allergy Asthma Immunol Res. 2016, 8:282-97.
-
Agarwal R1World J Radiol. Allergic bronchopulmonary aspergillosis: Lessons for the busy radiologist. 2011 Jul 28;3(7):178-81.



