A “gripping” case of myositis
Author: Matthew A. Christensen, MD, Resident Physician, University of Utah
Case
Intro: A 58 year-old woman with dermatomyositis diagnosed 4 months prior and treated with rituximab, mycophenolate, and steroids presented to the hospital with 3 days of dyspnea on exertion.
She had no pulmonary embolism, an infectious work-up was negative, and she continued to gradually worsen despite treatment with intravenous broad-spectrum antibiotics and ongoing work-up for 5 weeks.
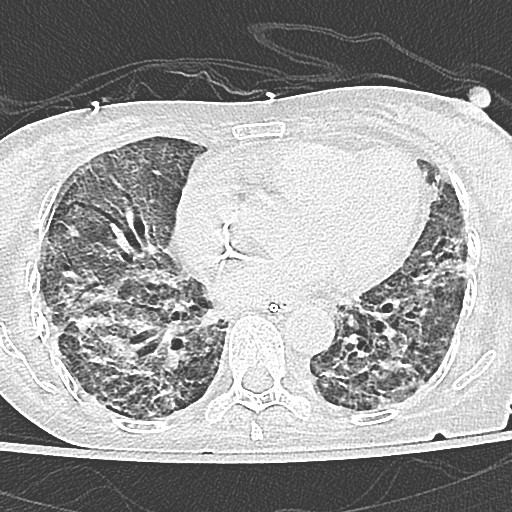
Image: A high-resolution CT chest was obtained
Question: What is the most likely etiology of this patient's respiratory failure?
- Development of dermatomyositis-associated ILD
- Atypical pneumonia in the setting of immunosuppression
- Aspiration causing lung injury
- Diffuse alveolar hemorrhage
The chest CT above demonstrates traction bronchiectasis, interstitial fibrosis and diffuse ground glass opacities consistent with a non-specific interstitial pneumonia (NSIP) radiographic pattern. This is most likely secondary to the development of interstitial lung disease in this patient with known dermatomyositis.
Discussion:
This patient presented with rapidly progressive interstitial lung disease (ILD) and hypoxic hypercarbic respiratory failure in the setting of a recent diagnosis of dermatomyositis (DM).
This high-resolution CT scan demonstrates several features of ILD:
- a reticular interstitial pattern with a mesh of overlapping linear opacities (e.g. right posterior portion)
- areas of ground glass opacities with a hazy appearance of preserved structures (e.g. anteromedial portions bilaterally)
- traction bronchiectasis with the "tram track" sign (e.g. right anterior portion) that results as the airways fail to taper in the periphery
This constellation of findings is consistent with NSIP, although there is considerable overlap in radiologic findings in ILD and other clinical data is needed for a complete diagnosis (1).
Bronchiectasis is defined as dilatation of the airways (bronchi = airways; ectasia = dilation of a tube). Fibrosis in ILD causes decreased parenchymal lung volumes and tissue retraction. The airways subsequently experience an "outward" pull resulting in traction bronchiectasis. In the absence of fibrosis and increased traction, bronchiectasis can occur by either increased pressure within the airways ("pulsion") or decreased structural integrity. For example, "pulsion" bronchiectasis can occur in allergic bronchopulmonary pneumonia as fungi and mucous fills the proximal airways; primary bronchial weakness with resultant bronchiectasis can be seen in Marfan syndrome (2). Cylindrical bronchiectasis is less likely to demonstrate airway obstruction compared to cystic bronchiectasis, although spirometric findings may vary (3)
ILD occurs in approximately 40% of patients with DM, although estimates vary from 20-80%. While DM-associated ILD usually progresses slowly, certain phenotypes can progress rapidly. This is particularly true in patients with amyopathic DM, which can result in substantial morbidity and mortality. The pathophysiology is poorly understood, with possible involvement of both cellular and humoral auto-immunity (4). Case series suggest that DM-ILD most frequently demonstrates an NSIP pattern on CT and biopsy (5).
Determining the etiology of dyspnea in patients with DM can be challenging. In addition to ILD other possibilities such as respiratory muscle weakness, drug-induced pneumonitis, and infection in the setting of immunosuppression must be considered. For this patient time was of the essence and five weeks of ongoing work-up may have precluded her from receiving more aggressive immunosuppressive therapy prior to respiratory failure, cardiac arrest, and death.
References:
-
Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: Glossary of Terms for Thoracic Imaging. Radiology 2008; 246:697–722.
-
Chan ED, Iseman MD. Bronchiectasis. In Broaddus VC, Mason RJ, Ernst JD, King TE, Lazarus SC, Murray JF, Nadel JA, Slutsky AS, Gotway MB, eds: Murray and Nadel's Textbook of Respiratory Medicine. Sixth Edition. Elsevier, 2016, pp. 853–876.
-
Alzeer A. HRCT score in bronchiectasis: Correlation with pulmonary function tests and pulmonary artery pressure. Ann Thorac Med 2008; 3:82.
-
Connors GR, Christopher-Stine L, Oddis C V, Danoff SK. Interstitial lung disease associated with the idiopathic inflammatory myopathies: what progress has been made in the past 35 years? Chest 2010; 138:1464–1474.
-
Douglas WW, Tazelaar HD, Hartman TE, Hartman RP, Decker PA, Schroeder DR, Ryu JH. Polymyositis-dermatomyositis-associated interstitial lung disease. Am J Respir Crit Care Med 2001; 164:1182–1185.



