Diagnosis needed STAT
Authors: Kenneth Chang, M.D 1, Mwelwa Chizinga, M.D 2, Divya C. Patel, D.O 2, Diana Gomez Manjarres, M.D 2
Department of Medicine; University of Florida
Division of Pulmonary, Critical Care, and Sleep Medicine; University of Florida
Case:
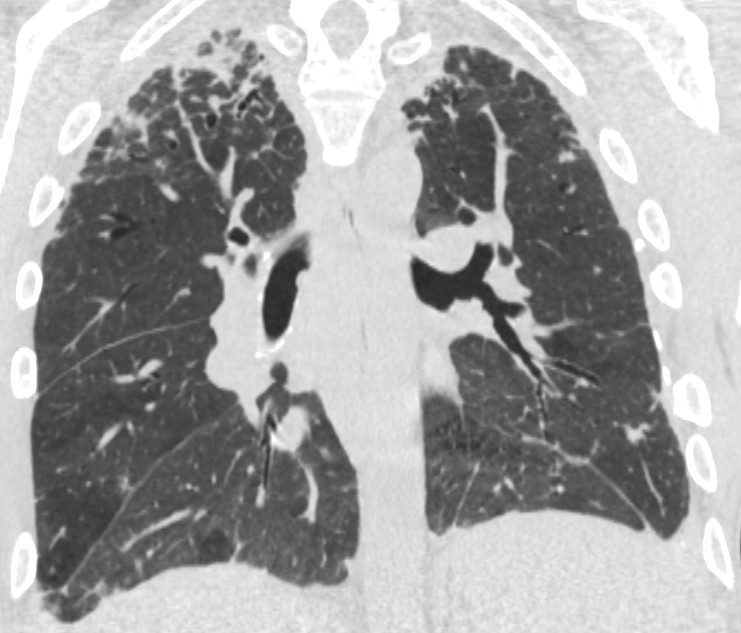
A 34-year-old Hispanic man presented to pulmonary clinic with progressive exertional dyspnea of two years duration. His medical history included childhood failure to thrive, recurrent sinus/respiratory infections, juvenile idiopathic arthritis, autoimmune hemolytic anemia and hypogammaglobulinemia. His work-up included lung function tests that revealed severe restrictive ventilatory defect (TLC 37% predicted) and severely reduced gas transfer (diffusion capacity of carbon monoxide 24% predicted). A high-resolution computed tomography (HRCT) of the chest showed mosaic attenuation with air trapping on expiratory images as well as areas of subpleural fibrosis and centrilobular nodules, and mediastinal lymphadenopathy.(Figure 1).
Question:
Which of the following tests is likely to yield a unifying diagnosis for this patient?
- Genetic testing
- Alpha 1 anti-trypsin level
- ACE level
- Immunoglobulin levels
- Hypersensitivity panel
A. Genetic Testing
Discussion:
Our patient had genetic testing which revealed an abnormal gain of function (GOF) mutation at the signal transducer and activator of transcription 3 (STAT3). The STAT family of transcription regulators is important for cellular proliferation, survival, and regulation of inflammation and autoimmunity. These mutations are inherited in an autosomal dominant manner and can occur as de novo or sporadic mutation. Clinical presentation of these patients is diverse and can be multi-systemic. Patients can develop autoimmune complications and immunodeficiency. Autoimmune complications include warm autoimmune hemolytic anemia, immune thrombocytopenia (ITP), diabetes, atopic dermatitis, hepatitis, autoimmune enteropathy, rheumatoid arthritis, and Interstitial lung disease (ILD). A recent series of 42 patients found that patients usually present early in life (average age 3 years) with the most frequent manifestations of disease being: autoimmune cytopenias (67%), lymphoproliferation (65%), enteropathy (57%), interstitial lung disease (36%), thyroiditis (31%), diabetes (24%), and postnatal growth failure (35%) (1). STAT3 GOF typically manifests with early endocrine and gastrointestinal disease, and hematologic disease and ILD present later in life.
Diagnosis is established by genetic testing. Currently there are ongoing randomized controlled trials to guide therapy in this condition. Targeted therapy such as anti-IL-6 receptor inhibitors (tocilizumab) with or without a JAK-inhibitor (ruxolitinib or tofacitinib) has been used with some benefit in small series (2). Immunoglobulin replacement therapy is indicated for patients with hypogammaglobulinemia. Avoidance of live vaccinations and genetic counseling are recommended.
In conclusion, STAT3 GOF syndrome is a newly described entity usually managed by hematologists and immunologists, but awareness amongst pulmonologists is paramount as these patients can present later in life with ILD and the diagnosis can be attained non-invasively.
References
-
Fabre, Alexandre, et al. “Clinical Aspects of STAT3 Gain-of-Function Germline Mutations: A Systematic Review.” The Journal of Allergy and Clinical Immunology: In Practice, vol. 7, no. 6, 2019
-
Forbes L, Vogel T, et al. Jakinibs for the treatment of immune dysregulation in patients with gain-of-function signal transducer and activator of transcription 1 (STAT1) or STAT3 mutations. Journal of Allergy and Clinical Immunology. Volume 142, Issue 5, November 2018, Pages 1665-1669



