Crazy Lungs
María A. Rodríguez-Santiago, MD 1
Elsie Cruz-Cuevas, MD 1
Mark A. Vergara-Gómez, MD 2
1University of Puerto Rico, School of Medicine, Internal Medicine Department
2University of Puerto Rico, School of Medicine, Division of Pulmonary and Critical Care Medicine
Case
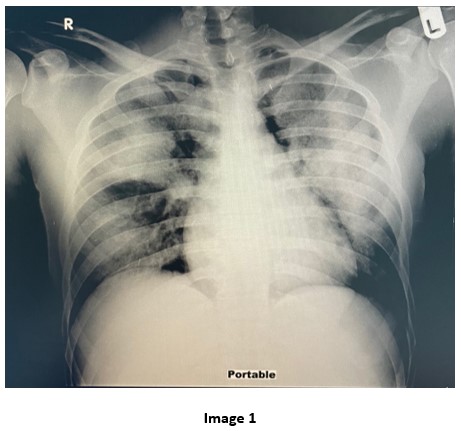
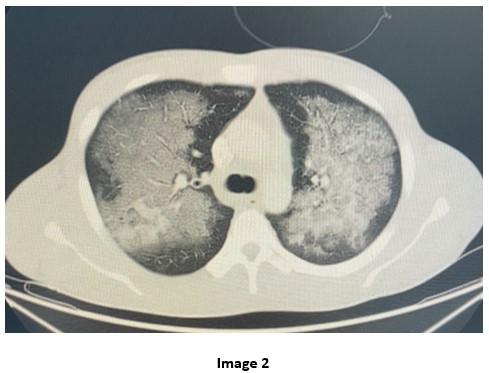
A 28-year-old male with Hepatitis C and history of substance abuse including synthetic marijuana and crack cocaine who presented with acute onset shortness of breath, hemoptysis and chest tightness of 2 hours duration. Upon evaluation, he was found to be hypoxic with SpO2= 80% on non-rebreather mask (FiO2= 100, Flow= 15L/min) requiring intubation. Complete Blood Count (CBC) revealed leukocytosis WBC= 21.13 x10 3 with neutrophilic predominance (92%) and left shifting of +1. Renal panel without major electrolyte disturbance or acid base disorders. The urine toxicology positive for Cocaine and THC. Mycoplasma IgM titers, Influenza A and B titers and Mycobacterium tuberculosis smear and culture were all negative. He was treated with systemic corticosteroid, scheduled bronchodilators and started on broad spectrum antibiotics. He was admitted to the Medical Intensive Care Unit. The chest X-ray and chest CT obtained are shown below
Question
Which of the following is the most likely causative agent of this patient’s abnormal radiological findings?
- IV drug cocaine
- Inhaled cocaine
- Synthetic Marijuana inhalation
- Reactivation of Pulmonary tuberculosis
- Aspiration pneumonia
B. Inhaled cocaine
Discussion
The Chest CT with contrast shows diffuse ground-glass opacities with interlobular septal thickening, also known as “Crazy-paving” pattern, with subpleural sparing in upper and lower lobes bilaterally attributed to cocaine inhalation (1). The combustion products, as well as the vasoconstrictive effect of inhaling crack-cocaine causes disruption in the pulmonary microvasculature leading to direct alveolar injury (2). Immunogenic response follows, as cocaine acts as an antigen that activates IgE and stimulates the release of histamine, serotonin and eosinophilic chemotactic factor causing direct lung injury (3). CT findings are non-specific and radiographically undistinguishable of other pulmonary eosinophilic diseases, non-cardiogenic pulmonary edema or diffuse alveolar hemorrhage (2). Cocaine is an alkaloid obtained from the leaves of a coca plant called Erythroxylon coca, it is widely abused and can result in a wide array of pulmonary changes. Crack cocaine is obtained when Cocaine hydrochloride (COC) is dissolved with hydrochloric acid (HCl) plus sodium bicarbonate and extracting it with ether, which makes it heat stable (1). Crack is not easily vaporized; therefore, it can be inhaled when smoked (2). Currently, the most widely used form of cocaine is crack because of its euphoric effects which are felt within minutes. Also, it is the most used illicit drug seen in hospital emergency departments (1). Smoking crack may induce a syndrome called Cocaine-induced eosinophilic lung injury or “crack lung” which is characterized by a cluster of symptoms including: fever, hypoxemia, hemoptysis, respiratory failure accompanied with the presence of diffuse alveolar damage, and hemorrhage with infiltrates rich in eosinophils. This syndrome usually occurs within 48 hours after smoking crack and resolves after its cessation (2). Pulmonary eosinophilia can be found on Bronchoalveolar lavage (BAL), as well as DAH, but in our case the patient left the medical facility against medical advice and the bronchoscopy could not be performed. The absence of peripheral eosinophilia as in our case does not rule out the diagnosis of “crack lung”. Our patient met the criteria for crack lung, including: (a) admitting to recently smoking cocaine, (b) typical chest CT with ground-glass opacities with subpleural sparing, and (c) rapid improvement after offending drugs was removed. In view of the increasing incidence and prevalence of cocaine-induced pulmonary disease, crack lung should be immediately added to the differential diagnosis, rather than being a diagnosis of exclusion in the correct scenario. Treatment for crack lung is mainly supportive, although some cases have reported using systemic glucocorticoids for 2 weeks after resolution of symptoms (2). Intravenous cocaine users are more likely to develop bacterial pneumonia and septic emboli, which would appear as peripherally round opacities that may cavitate (1) (Answer choice A is incorrect). The CT findings for Synthetic marihuana are diffuse miliary micronodular pattern and tiny centrilobular nodules in tree-in-bud configuration (4) (Answer choice C is incorrect). Reactivation of pulmonary tuberculosis usually appears with centrilobular small nodules and upper lobes patchy consolidation with or without cavitations (5) (Answer choice D is incorrect). Aspiration pneumonia shows involvement of the dependent portions of the lung in the supine position (1) (A nswer choice E is incorrect).
References
-
Restrepo C, Carrillo J, Martinez S, et. al. Pulmonary Complication from Cocaine and Cocaine-based Substances: Imaging Manifestations. RG. 2007; 27(4): 941-956. Doi: 10.1148/rg.274065144
-
Rocha de Almeida R, Zanetti F, Soares A, et al. Cocaine-induced Pulmonary Changes: HRCT Findings. J Bras Pneumol. 2015;41(4):323-330. Doi: https://doi.org/10.1590/S1806-37132015000000025
-
Shanti C and Lucas C. Cocaine and the Critical Care Challenge. Crit Care Med. 2003;31(6):1851-1859. Doi: 10.1097/01.CCM.0000063258.68159.71
-
Berkowitz E, Henry T, Veeraraghavan S, et. al. Pulmonary Effects of Synthetic Marijuana: Chest Radiography and CT Findings. AJR. 2015;204(1):750-757. Doi: 10.2214/AJR.14.13138
-
5Kim J, Jae-Lee I, Kim J. CT Findings of Pulmonary Tuberculosis and Tuberculous Pleurisy in Diabetes Mellitus Patients. Diagn Interv Radiol. 2017;23(1):112-117. Doi: 10.5152/dir.2016.16157