Achy Breaky Heart
J Saadi Imam MD PhD, Shawn P Nishi MD
Division of Pulmonary, Critical Care, and Sleep Medicine, Department of Internal Medicine,
The University of Texas Medical Branch at Galveston, TX
Case
A 56-year-old obese female with necrotizing fasciitis requiring multiple debridements developed acute onset hypoxia, altered mentation, anuric renal failure and shock requiring vasopressors on day 25 of her hospitalization. She had been receiving antibiotics, argatroban (due to concern for heparin-induced thrombocytopenia), and IV fluids when she decompensated and was too unstable to transport for imaging studies. Pulmonary medicine was consulted to evaluate for management of suspected pulmonary embolism after bedside transthoracic echocardiogram and chest x-ray were performed showing preserved EF, severely dilated RV and mild cardiomegaly.
Vital Signs: BP 73/24 mmHg, Pulse 98 beats/min, T 38.4 °C, Resp 21/min, Wt 137.3 kg (92 kg admission), SpO2 98%
Physical Examination: 3+ upper and lower extremity pitting and dependent edema.
Arterial blood gas: pH7.39/PaO2 324mmHg/PCO2 33mmHg/HCO3 20 mmol/L on 100% FiO2
NT-proBNP level 3540 pg/mL; cardiac enzymes were normal
EKG: Normal, sinus rhythm
Lower extremity Doppler ultrasound: negative for DVT
Transthoracic echocardiogram 10 days prior (Video 1) and now (Video 2).
Imaging
Video 1
Video 2
Question
Based on the echocardiogram findings and clinical presentation, what is the most likely diagnosis?
- Left ventricular systolic failure from septic cardiomyopathy
- Right ventricular failure from volume overload
- Hyperdynamic left ventricular outflow obstruction
- Bacterial endocarditis
Answer: B. Right ventricular failure from volume overload
Discussion
On chart review, the patient was found to be 28 L positive with a 100 lb increase in her documented weight since admission. On exam, she had clear signs of volume overload with anasarca and JVD. Her hemodynamic instability with vasopressor requirement and echocardiogram findings of severe RV dilatation and flattened interventricular septum were consistent with RV pressure/volume overload.
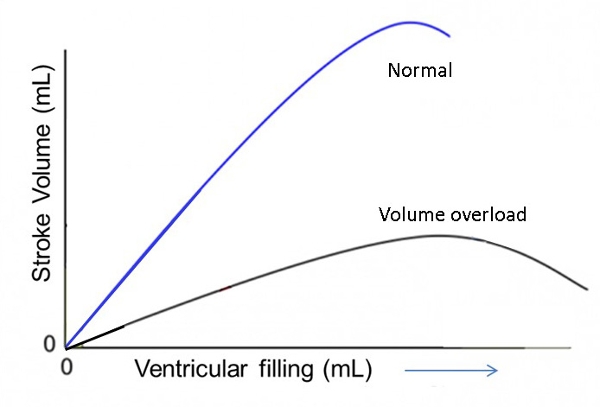
In this case, despite the RV’s relatively high compliance, acute volume overload led to RV dilatation. The RV function is represented by the points on the descending part of the Frank-Starling curve associated with decreased RV stroke volume and cardiac output. This is due to elevated RV end-diastolic volume and reversal of the ventricular septal gradient as seen by septal flattening. Clinically, this manifests as a shock state.
Although massive pulmonary embolism can yield a similar presentation, the patient had been anticoagulated for several days prior to her decompensation and lower extremity Dopplers were negative. While negative DVT studies cannot definitively rule out the presence of a PE, the development of PEs while on therapeutic anticoagulation is a rare occurrence with a prevalence of 1.2% in a recent study published by Liu et al.,2018. Regardless, the patient was continued on argatroban therapy during the remainder of her hospitalization. Over the next 3 days, >14 L ultrafiltrate were removed and the patient was rapidly weaned off pressors and extubated to room air. Transthoracic echo did not show evidence of valvular vegetations, LV systolic failure or demonstrate LV outflow tract obstruction from a hyperdynamic LV, making these choices less likely.
References
-
Matthews JC, McLaughlin V. Acute right ventricular failure in the setting of acute pulmonary embolism or chronic pulmonary hypertension: a detailed review of the pathophysiology, diagnosis, and management. Curr Cardiol Rev 2008; 4(1): 49-59.
-
Cecconi M, Johnston E, Rhodes A. What role does the right side of the heart play in circulation? Crit Care 2006;10(Suppl 3): S5.
-
Mebazaa A, Karpati P, Renaud E, Algotsson L. Acute right ventricular failure--from pathophysiology to new treatments. Intensive Care Med 2004; 30(2):185-196.
-
Lahm T, McCaslin CA, Wozniak TC, et. al. Medical and surgical treatment of acute right ventricular failure. J Am Coll Cardiol 2010; 56(18):1435-46.
-
Walker LA, Buttrick PM. The right ventricle: biologic insights and response to disease: updated. Curr Cardiol Rev 2013; 9(1): 73-81.
-
Liu MY, Ballard DW, Huang J, et. al. Acute pulmonary embolism in emergency department patients despite therapeutic anticoagulation. West J Emerg Med 2018; 19(3): 510-516.



