A CT Finding No Longer Zebra-Specific
Jared Johnstun, MD
Pulmonary and Critical Care Medicine Fellow
University of Utah School of Medicine
Case
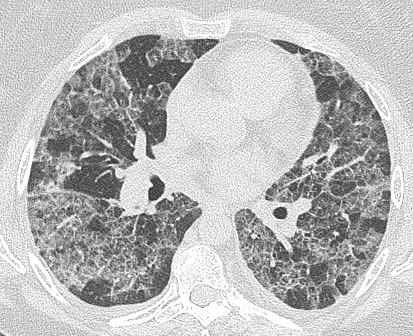
A 54 year old woman presented to the emergency department for shortness of breath after 72 hours of fever, chills and a cough productive of yellow sputum. She was severely hypoxemic with a PaO2 of 36mmHg on room air. Aside from a serum sodium level of 125mmol/L, the remainder of her labs were unremarkable. A chest X-ray showed diffuse alveolar opacities and a subsequent high-resolution CT scan is shown below.
Clinical Question
What is the radiographic finding, and what disease is this finding specific for?
Crazy-paving. The differential diagnosis for the “crazy-paving sign” is actually quite large and goes well beyond Pulmonary Alveolar Proteinosis (PAP). Although the majority of patients with PAP will have a CT consistent with the crazy paving pattern, this radiographic pattern is by no means specific to PAP. Crazy-paving can be seen in a variety of much more common disease states, thus the overall incidence of the finding will be seen more frequently in the more common disease processes.
Discussion
Crazy-paving on CT refers to the findings of ground-glass opacities (patchy or diffuse) with thickened interlobular septae and intralobular lines. It gets its name from the similar appearance to a pathway made up of disorganized paving-stones.1-6

Crazy Paving: Public Domain Image, credit Liam Quin
Originally described in 6 case reports from 19895, the crazy-paving pattern on chest CT scan was thought to be specific to alveolar macrophage dysfunction resulting in the pulmonary disease known as Pulmonary Alveolar Proteinosis, or PAP. The exact causes for the radiographic findings that make up crazy paving turns out to be as diverse as the differential diagnosis. This finding is detected more commonly now with newer multidetector CT scans with better image resolution.
The linear component may be caused by thickened interlobular septae, thickened intralobular septae, distal airspace compaction and/or intralobular interstitial thickening.3 The ground glass opacities (GGOs) represent partially filled alveoli (edema, inflammatory cells, blood and/or proteinaceous exudates), thickened alveolar walls and/or thickening of the surrounding interstitium.3,4 In PAP, the GGOs reflect alveoli partially filled with periodic acid Schiff positive lipid rich fluid and the linear component reflects interlobular and interstitial inflammation. 4,5 In heart failure, the linear component and GGOs reflect hydrostatic edema infiltrating the alveoli, septae and interstitium.6
Although the majority of patients with PAP will have a CT consistent with the crazy-paving pattern it is by no means specific4 and it is actually seen more frequently in disease states other than PAP (Table 1). It is important to recognize that this image finding is nonspecific and likely warrants further diagnostic evaluation.
Common causes of crazy paving1-7
- Acute Respiratory Distress Syndrome (ARDS)
- Bacterial Pneumonia
- Acute Interstitial Pneumonia (AIP)
- Pneumocystis Jerovecii pneumonia (PJP)
- Mucinous Bronchoalveolar Carcinoma
- Chronic Aspiration
- Lipoid Pneumonia
- Viral Pneumonia
- Fungal Pneumonia
- Pulmonary Alveolar Proteinosis (PAP)
- Granulomatosis with Polyangitis
- Microscopic Polyangitis
- Churg-Strauss Syndrome
- Goodpastures Disease
- Collagen vascular diseases
- Idiopathic hemorrhage
- Mycoplasma pneumonia
- Non-specific Interstitial Pneumonia (NSIP)
- Alveolar Sarcoidosis
- Chronic Eosinophilic Pneumonia
- Acute Usual Interstitial Pneumonia (UIP)
- Cryptogenic Organizing Pneumonia (COP)
- Drug induced pneumonitis
- Pulmonary Veno-Occlusive Disease (PVOD)
- Pulmonary edema
- Radiation Pneumonitis
- Graft-vs Host Disease
- Lymphangitic Carcinomatosis
- Hypersensitivity Pneumonitis
The patient received mechanical ventilation and underwent diagnostic bronchoscopy. Neither gross findings nor lavage (80% neutrophils, 10% macrophages and 10% respiratory epithelial cells) showed evidence of proteinosis. Subsequent wedge resection biopsy demonstrated peribronchial lymphohistiocytic infiltrates, extensive alveolar septal involvement, immature collagen matrix formation, and pigmented macrophages in the alveolar spaces. These were deemed most consistent with cryptogenic organizing pneumonia in an active smoker. The patient was treated with corticosteroids and demonstrated rapid improvement.
Resources
-
Maimon N, Heimer D. The crazy-paving pattern on computed tomography. CMAJ. 2010;182:1545
-
Rossi S, Erasmus J, Volpacchio M, et al. “Crazy-Paving” Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview. Radiographics. 2003; 23:1509-1519
-
De Wever W, Meersschaert J, Coolen J, et al. The crazy-paving pattern: a radiological-pathological correlation. Insights Imaging 2011; 2:117–132
-
Murch CR, Carr DH. Computed tomography appearances of pulmonary alveolar proteinosis. Clin Radiol 1989;40:240–243.
-
Lee, CH. The Crazy-paving Sign. Radiology. 2007;243:905-906.
-
Senturk A, Karalezli A, et al. A Rare Cause of Crazy Paving and Mediastynal Lymphadenopathy: Congestive Heart Failure. J Clin Imag Sci. 2013; 3:1-4
-
Johkoh T, Itoh H, Müller NL, et al. Crazy-paving appearance at thin-section CT: spectrum of disease and pathologic findings. Radiology 1999;211:155-60.



