A Coin in the Lung
Bonnie R. Wang, MD1, Aamer Chughtai, MD2, Amir Lagstein, MD3, Jakob I. McSparron, MD1
1Division of Pulmonary and Critical Care, University of Michigan, 2Department of Radiology, University of Michigan, 3Department of Pathology, University of Michigan
Case
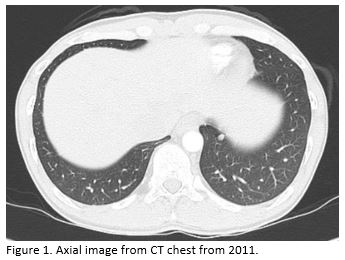
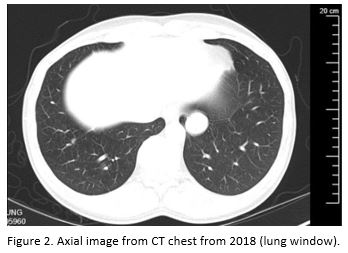
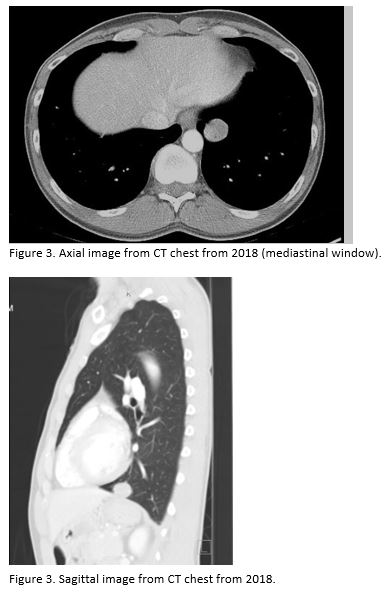
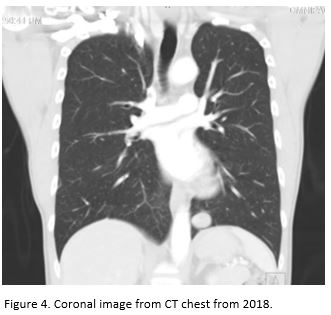
A 42-year-old daily cigarette and marijuana smoker presented to an Emergency Department with four months of progressive shortness of breath. Representative slices of chest CT scan with contrast compared to a prior CT scan 7 years ago are shown below. The patient subsequently underwent a CT-guided biopsy, and the results are also shown below.
Question
Which of the following is most likely?
A. Infectious granuloma.
B. Hamartoma.
C. Rounded atelectasis.
D. Granulomatosis with polyangiitis.
E. Carcinoid.
B. Hamartoma
Discussion
Hamartomas are the most common benign lung neoplasms and are often incidentally discovered on imaging. They are generally found in adults, with a higher male predominance. The most common radiologic pattern of a hamartoma is a solitary lung nodule that appears like a coin lesion in the periphery of the lung. Hamartomas are solid, and the majority are <4 cm, and appear round with smooth, clearly delineated margins. Endobronchial hamartomas account for 10-25% of cases.
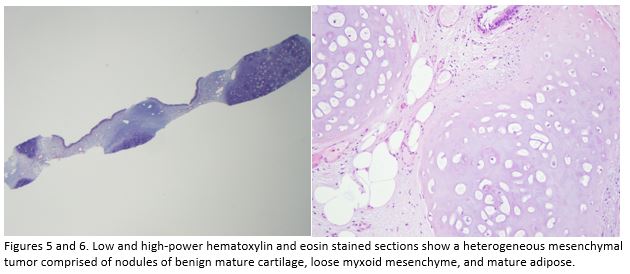
Typical radiographic features of pulmonary hamartomas include popcorn calcification or intranodular fat (-40 to -120 HU). These features may be absent approximately 30% of the time, requiring biopsy or resection for definitive diagnosis. PET/CT findings can be supportive, but hamartomas (especially those larger in size) can have uptake characteristics that suggest malignancy. Histologic examination reveals a mixture of cartilage, fat, smooth muscle, myxomatous connective tissue, bone, and clefts lined by respiratory epithelium.
The association between pulmonary hamartomas and malignancy is controversial. There are observational studies describing an increased risk of bronchial cancer, and case reports of patients with hamartomas and synchronous malignancy. Most pulmonary hamartomas are non-expanding or slow-growing. Surveillance is recommended, and surgical resection can be considered in hamartomas greater than 2.5cm in size, rapidly expanding nodules, uncertainty in diagnosis or difficulty differentiating from malignancy, or if patients are symptomatic.
While granulomas can be round, solid and solitary, the patient had no clinical signs or symptoms of infection (A). Rounded atelectasis (C) is usually subpleural with a characteristic comet tail sign and adjacent pleural thickening. Nodules or masses suggestive of granulomatosis with polyangiitis (D) are often multiple and can appear densely consolidated, cavitary, or with surrounding ground glass. A carcinoid tumor of the lung (E) could be considered as these are commonly incidentally found solitary nodules, but the histopathologic result is not consistent.
References
-
Myers, JL. Lung. Rosai and Ackerman's Surgical Pathology, 1: 372-443.
-
De Cicco, C., et al. Imaging of lung hamartomas by multidetector computed tomography and positron emission tomography. Ann of Thorac Surg 2008; 86: 1769-72.
-
Huang, Y., et al. CT- and computer-based features of small hamartomas. Clin Imaging 2011; 35: 116-22.
-
Ekinci, G.H., et al. The frequency of lung cancer in patients with pulmonary hamartomas: An evaluation of clinical, radiological, and pathological features and follow-up data of 96 patients with pulmonary hamartomas. Rev Port Pneumol 2006; 23: 280-286.
-
Elsayed, H., et al. Is resection necessary in biopsy-proven asymptomatic pulmonary hamartomas? Interactive CardioVascular and Thoracic Surgery 2015; 21: 773-776.



