Case Editor - Victor Kim
Reviewed By Environmental & Occupational Health Assembly
Submitted by
Erica Hughes, MD
Senior Pulmonary Fellow
University of Texas Southwestern Medical Center
Dallas, Texas
Craig Glazer, MD, MSPH, FCCP
Assistant Professor of Medicine
University of Texas Southwestern Medical Center
Dallas, Texas
History
A 51-year-old man initially presented with dyspnea and dry cough. He denied any constitutional symptoms including fevers, chills, arthralgias, myalgias, night sweats and weight loss. His primary care physician initially treated him with antibiotics without response. The dyspnea on exertion and cough continued to progress over the next several months.
His past medical and surgical history was unremarkable. His family history was positive for sarcoidosis. He was taking no medication and was a nonsmoker. He had no allergies. His occupational history was significant for working in a hospital for many years, and he was not exposed to workplace agents associated with interstitial lung disease.
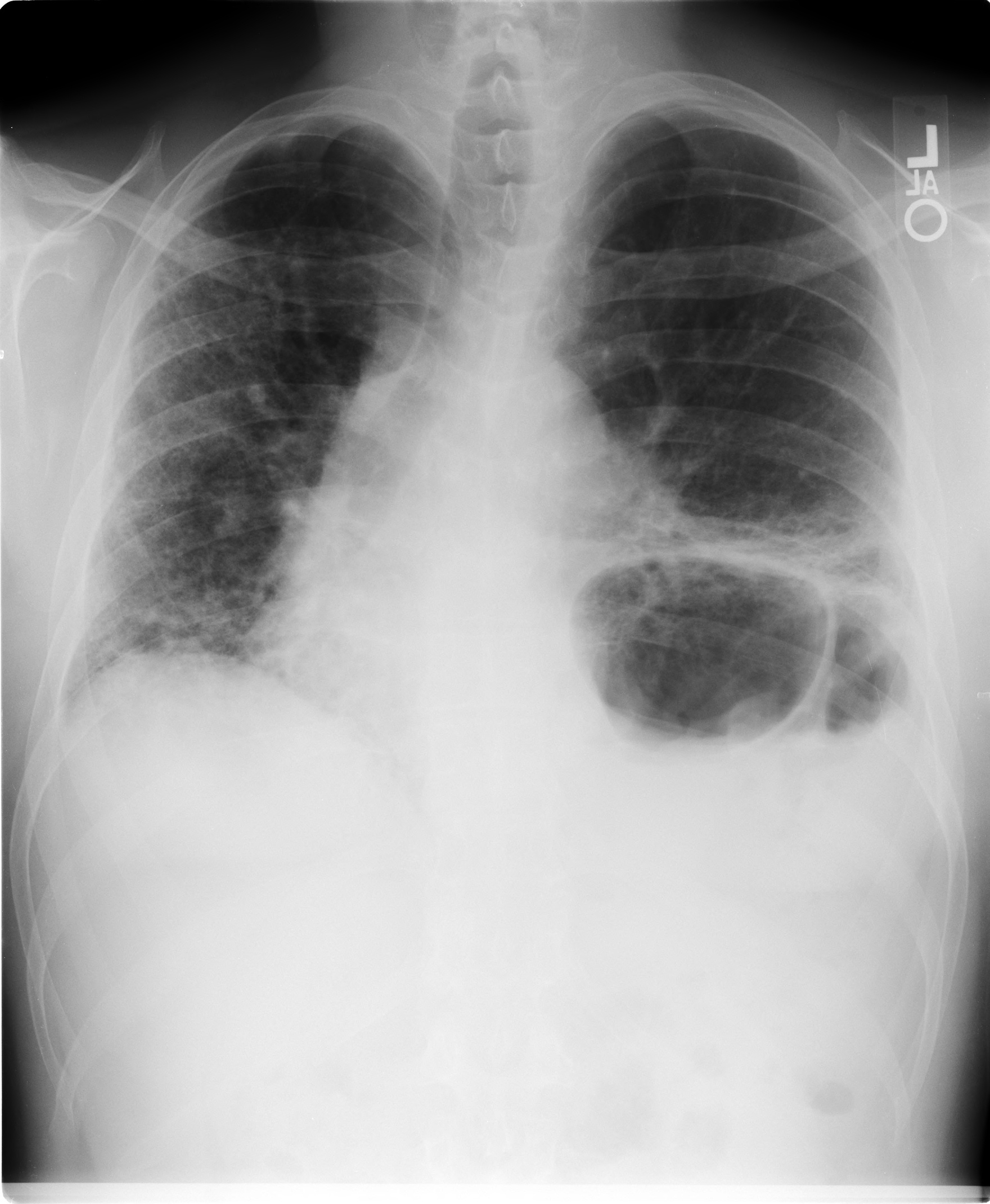
After several months of symptoms unresponsive to antibiotics, a chest radiograph was performed and revealed interstitial disease. He was subsequently referred to a pulmonologist who performed pulmonary function tests that showed restriction and a severely reduced diffusion capacity.
Physical Exam
Vital Signs
temperature 36.7°C
respiration 20
pulse 120
blood pressure 126/87
oxygen saturation 92% (room air)
Although tachypneic, he was not using his accessory muscles. HEENT was unremarkable. Chest examinations indicated symmetric excursions and expansion, resonant to percussion bilaterally. There were bilateral inspiratory crackles halfway up the chest posteriorly. His heart rhythm was regular and he had no murmur or gallop. His abdomen was soft with normal bowel sounds and no organomegaly. His extremities were without cyanosis, clubbing or edema. His skin and joint exams were unremarkable.
Lab
Pulmonary function tests
FVC 2.44 (51%)
FEV1 2.07 (54%)
FEV1/FVC 0.85
DLCO 26% predicted
TLC 3.53 (45%)
A high-resolution computed tomography (HRCT) of the chest showed diffuse ground-glass opacities with bibasilar fibrotic changes. A bronchoscopy with bronchoalveolar lavage and transbronchial biopsy revealed 30% lymphocytes and nondiagnostic pathology. An open lung biopsy revealed fibrotic nonspecific interstitial pneumonia (NSIP). Prednisone was started with some initial symptomatic improvement. His symptoms, however, progressed again despite continued prednisone, and he was referred to our institution for a second opinion. At the time we evaluated him, his symptoms were present 1 year and had continued to progress despite the treatment with prednisone. His physical examination revealed diffuse inspiratory crackles and he required continuous supplemental oxygen because of resting hypoxemia.
His connective tissue serologies were negative, but on further questioning, he admitted buying two parakeets for his family 3 months before the onset of symptoms. Precipitins to parakeet droppings were negative. The birds were removed from his home, and his house, including the heating and air conditioning system, was professionally cleaned. The house had no carpet in the area where the birds were housed. Azathioprine was added to his prednisone, starting at 50 mg/day with plans to increase the dose over a 2 month period if needed. One month later, his symptoms were markedly improved and his supplemental oxygen was discontinued. His prednisone and azathioprine were weaned over the next year. He is now stable off all therapy.
Figures
References
- Katzenstein AA, Fiorelli R.F. Nonspecific Interstitial Pneumonia/Fibrosis. Am J Surgical Pathology 1994; 18: 136-147.
- Cormier Y. Hypersensitivity Pneumonitis. In: Rom W, ed. Environmental & Occupational Medicine, 3rd ed. Philadelphia: Lippincott-Raven, 1998:457-466.
- Travis WD, Colby TV, Koss MN, et al., Non-Neoplastic Disorders of the Lower Respiratory Tract. Washington D.C. American Registry of Pathology and the Armed Forces Institute of Pathology.
- Vourlekis J, Schwarz MI, Cool CD, et al., Nonspecific Interstitial Pneumonitis as the Sole Histologic Expression of Hypersensitivity Pneumonitis. Am J of Medicine 2002; 112: 490-493.
- Ohtani Y, Saiki S, Kitaichi M, et al., Chronic bird fancier’s lung: histopathological and clinical correlation. An application of the 2002 ATS/ERS consensus classification of the idiopathic interstitial pneumonias. Thorax 2005; 60:665-671.
- Reyes CN, Wenzel FJ, Lawton BR, et al., The Pulmonary Pathology of Farmer’s Lung Disease. Chest 1982;81:142-146
- Churg A, Muller NL, Flint J, et al., Chronic Hypersensitivity Pneumonitis. Am J Surg Pathol 2006;30:201-208.
- Lynch DA, Newell JD, Logan PM, et al., Can CT Distinguish Hypersensitivity Pneumonitis from Idiopathic Pulmonary Fibrosis? AJR Am J Roentgenol 1995;165:807-812.
- Cormier Y, Letourneau L, Racine G. Significance of precipitins and asymptomatic lymphocytic alveolitis: a 20 year follow-up. Eur Resp J 2004;23:523-525.
- Cormier Y, Belanger J, LeBlanc P, et al., Bronchoalveolar lavage in farmer’s lung disease: diagnostic and physiologic significance. Br J Ind Med 1986;43:401-405.
- Fink JN, Ortega HG, Reynolds HY, et al. Needs and Opportunities for Research in Hypersensitivity Pneumonitis. NHLBI/ORD Workshop. Am J Respir Crit Care Med 2005;171:792-798.
- Lacasse Y, Selman M, Costabel U, et al., Clinical Diagnosis of Hypersensitivity Pneumonitis. Am J Respir Crit Care Med 2003;168:952-958.
- Rose C. Hypersensitivity Pneumonitis. In: Murray JF NJ, ed. Textbook of Respiratory Medicine. 3 ed. Philadelphia: W.B. Saunders Company; 2000:1867-1884.
- Schmidt CD, Jensen RL, Christensen LT, et al., Longitudinal pulmonary function changes in pigeon breeders. Chest 1988;93:359-363.
- Cormier Y, Belanger J. Long-term physiologic outcome after acute farmer's lung. Chest 1985;87:796-800.
- Barbee RA, Callies Q, Dickie HA, et al., The long-term prognosis in farmer's lung. Am Rev Respir Dis 1968;97:223-231.
- Yoshizawa Y, Miyake S, Sumi Y, et al. A follow-up study of pulmonary function tests, bronchoalveolar lavage cells, and humoral and cellular immunity in bird fancier's lung. J Allergy Clin Immunol 1995;96:122-129.
- Bourke SJ, Banham SW, Carter R, et al. Longitudinal course of extrinsic allergic alveolitis in pigeon breeders. Thorax 1989;44:415-418.
- Craig TJ, Hershey J, Engler RJ, et al., Bird antigen persistence in the home environment after removal of the bird. Ann Allergy 1992;69:510-512.
- Kokkarinen JI, Tukiainen HO, Terho EO. Effect of corticosteroid treatment on the recovery of pulmonary function in farmer's lung. Am Rev Respir Dis 1992;145:3-5.
- Monkare S. Influence of corticosteroid treatment on the course of farmer's lung. Eur J Respir Dis 1983;64:283-293.