and
J.M.Joshi, M.D.
Professor and Head, Department of Respiratory Medicine
T.N. MedicalCollege & B.Y.L. Nair Charitable Hospital
Mumbai, India
Case Presentation:
A 62-year-old man, retired shipping company employee, who was to undergo resection of a vocal cord nodule, was referred to the Chest clinic for preoperative evaluation for an abnormal chest radiograph (Figure 1).
Click on images to enlarge.
Figure 1: Chest radiograph on presentation showing bilateral interstitial shadows, pleural plaques and diffuse pleural thickening.
A detailed history revealed exertional dyspnoea without wheezing, and dry cough for the last two years. He admitted to a 45-pack year history of smoking. He had worked as a repair and maintenance worker in a shipping company for 25 years and had retired from work for a year before this assessment. During the last 3 years of work, he was also involved in loading raw mine ore onto the ships. He was not aware of the exact nature of the ore.
On examination, he had clubbing of the fingers. Respiratory system examination showed bibasilar fine inspiratory crackles.
His laboratory investigations revealed hemoglobin of 14.5 gm/dL, a white blood cell count of 5,800/mm3 with differential count showing neutrophils - 56%, lymphocytes - 40% and eosinophils - 4%. Arterial blood gases on room air showed pH of 7.37, PaO2 of 78mm Hg, PaCO2 of 43 mm Hg, and HCO3 of 26 mmols/L. Pulse oximetry showed a saturation of 93% at rest and decreased to 89% with exercise on room air. The biochemical profile and urine examination was normal. Spirometric results are shown in Table 1.
Table 1: Spirometric results on presentation.
|
Predicted |
Pre-bronchodilator (Observed/Predicted) |
Post-bronchodilator (Observed/Predicted) |
|
|
FVC |
3.52 L |
1.73 (49%) |
1.84(52%) |
|
FEV1 |
2.76 L |
1.27(46%) |
1.34(48%) |
|
FEV1/FVC |
79% |
74% |
73% |
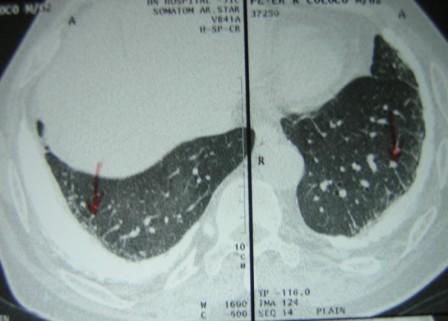
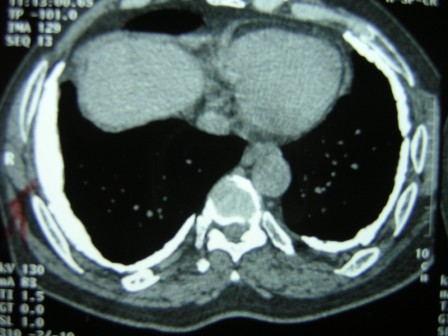
High Resolution CT scan of the lungs (Figure 2) showed bilateral pleural plaques, diffuse pleural thickening and increased interstitial markings. These changes were confirmed on prone films as well. (Figure 3) The calcified pleural plaques are particularly well seen on the mediastinal window of the CT scan (Figure 4).
Figure 3:High Resolution CT scan of the lungs in prone position.
Figure 4: CT scan of the thorax — mediastinal windows.
On the basis of his occupational history and radiological findings, he was diagnosed to have asbestos-induced pleuroparenchymal disease. A two-dimensional echocardiogram showed resting pulmonary arterial pressure of 50 mm Hg with dilated right atrium and right ventricle and normal left ventricular function.
He subsequently underwent vocal cord nodule excision uneventfully. The pathology of the excised nodule showed benign squamous papilloma.
Question 1:
In this case, which of the following options is LEAST likely to be due to asbestos exposure?
a. Pleural Thickening
b. Pleural Plaques
c. Interstitial lung disease
d. Vocal cord nodule
e. Pulmonary hypertension..
The correct answer is d.
Asbestos exposure is known to cause diffuse and circumscribed pleural thickening (the latter synonymous with pleural plaques) and interstitial pneumonitis and fibrosis (asbestosis). The risk of cancer of the larynx is increased with asbestos exposure [1]but there is no known association of benign vocal cord nodules and asbestos exposure. This finding was incidental in this patient. The pulmonary hypertension although not directly caused by the asbestos fibers, is secondary to the asbestosis.
Question 2:
Which of the following is LEAST useful clinically in diagnosing asbestosis?
a. Occupational history and clinical examination
b. Radiological features
c. Bronchoalveolar lavage (BAL) for asbestos bodies
d. Open lung biopsy and measurement of quantitative fiber content in lung tissue
e. C and D
The correct answer is e.
Occupational history of exposure to asbestos in the presence of classic clinical and radiological features strongly supports the diagnosis of asbestos-induced lung disease. The history may not be accurate, however, as patients may often not know that they have been exposed to asbestos at work or elsewhere. It may be helpful for the clinician to keep in mind workplaces which may involve asbestos exposure such as thermal insulation, construction and demolition work, electrical work, shipyard work and manufacture of asbestos cement and friction products. It is also important to remember the long latent period, which is often decades until disease develops after asbestos exposure. Hence the patient should be carefully interviewed regarding all his past occupations.
On chest radiography, pleural plaques when calcified and bilateral (as in this case) are the most common indicators of inhalation, retention and biologic effect of asbestos fibers [2].
Most asbestos fibers remain uncoated and are therefore invisible on light microscopy due to their size. Asbestos bodies usually form around amphibole fibers, but may occasionally form around other non-asbestos fibrous particles too, which means they are not specific for asbestosis either [3].
BAL cells can also be digested with bleach and the residue examined by electron microscopy, with fibers expressed per 10 6 alveolar macrophages. The recovery of fibers is higher in those exposed to asbestos versus those who are not. However this relation only holds good for amphibole fibers and not for the chrysolite variety as the latter undergo translocation, clearance and dissolution due to their physical properties [4].The number of fibers in the lung can also be assessed in open lung biopsy specimens by electron microscopy or phase contrast microscopy. However cost, limited availability, and invasiveness do not make these tests a practical option in the clinical setting. There is also a great deal of variability amongst different laboratories.
Question 3:
Which ONE of the following statements describing association of smoking and asbestos induced lung disease is NOT true?
a. Smoking increases the risk of lung carcinoma in persons exposed to asbestos.
b. Smoking plays no role in the prevalence of pleural plaques.
c. Smoking is a confounding factor when determining the relation of lung cancer and asbestos exposure.
d. Smoking causes increased retention of asbestos fibers in the lung.
e. In lung cancer patients with a positive history of asbestos exposure, lower lobe predominant tumor and adenocarcinomas are more common.
The correct answer is e.
Asbestos exposure and smoking multiply the risk of lung carcinoma [5].Thus, if a smoker has a risk of lung cancer ten times that of a non-smoker and someone exposed to high levels of asbestos five times the risk of someone not exposed to asbestos, then someone who both smokes and is exposed may have up to fifty times the risk of a non-exposed non-smoker. Also in patients with lung cancer who are smokers and have been exposed to asbestos, the apportionment of blame to asbestos as the causative factor of cancer becomes difficult.
Smoking plays no role in the prevalence of pleural plaques [6].Cigarette smoking causes enhanced retention of bothamosite and chrysotile in the airway mucosa and may thus potentiate the pathologic effects of asbestos [7].
At first glance, Statement e seems rational considering that asbestosis occurs in the lower lobes and the fibrosed and scarred lung may predispose to scar carcinoma (adenocarcinoma). Initial studies also supported this theory, but these did not adequately adjust for potential confounders such as the patient's age, sex, race, and family history of cancer. However, recent studies have concluded that smoking and asbestos exposure history both favor an upper lobe location of tumor and asbestos exposure does not influence the tumor histology [8].
Question 4:
Which of the following statements is MOST appropriate to counsel this patient as regards his prognosis?
a. 'Prognosis is excellent, there is nothing to worry about as long as you continue to be a non-smoker'.
b. 'Prognosis is dismal as you have extensive pleural disease'
c. 'Prognosis is dismal as you have both pleural and parenchymal disease'.
d. 'Prognosis is dismal as your lung function is abnormal and there is nothing, which can reverse this'.
e. 'Prognosis is guarded, follow-up is necessary to monitor for progression of established disease'.
The correct answer is e.
The patient should be informed that the disease is due to occupational asbestos exposure and has involved the pleura and parenchyma and may progress. The risk of lung cancer and mesothelioma and the multiplicative effect of smoking should also be emphasized so that smoking cessation is reinforced. Despite the moderate to severe reduction in pulmonary function, his excellent functional status coupled with his abstinence from smoking, may afford him a guarded prognosis. Follow-up with chest radiography and pulmonary function testing every three to five years is necessary to monitor for progression of established disease [2].
Question 5:
Which of the following asbestos fibers cause mesothelioma?
a. Chrysolite
b. Crocidolite
c. Amosite
d. Tremolite
e. All of the above
The correct answer is e.
Asbestos fibers are of two types: the serpentine (chrysolite) and the amphibole variety (crocidolite, amosite, tremolite, anthophyllite and actinolite). All asbestos fibers are associated with an increased risk of mesothelioma. The risk may be higher with amphiboles compared to serpentines and the highest with crocidolite followed by amosite. It is believed that amphiboles being short, straight fibers with reduced clearance from the body can be retained indefinitely, penetrate the interstitium of the distal lung and show extensive mobility both in the lungs and around the body. The risk of developing mesothelioma may also be dose-related. Hence high-dose chrysolite fibers may be more likely to result is mesothelioma then low-dose or incidental exposure to crocidolite.
Mesothelioma has also been described in people living in various parts of rural Turkey. In one of these regions where mesothelioma was endemic, tremolite asbestos was extensively used as building and white wash material as it was naturally available in the soil [9]. In another region in Turkey, a non-asbestos mineral, fibrous erionite was thought to be the cause [10].This observation suggests that the propensity of minerals to cause mesothelioma may be due to their physical rather than their chemical properties. This raises concerns over the long-term safety of fibrous substitutes for asbestos. It may therefore be prudent to minimize the use of very fine fibers within the respirable range irrespective of their chemical properties.
COMMENTS: Please send any comments to S. Bhat, M.D.
SUGGESTED RESOURCES:
REFERENCES:
- Seidman, H., I.J. Selikoff, and S.K. Gelb, Mortality experience of amosite asbestos factory workers: dose-response relationships 5 to 40 years after onset of short-term work exposure. Am J Ind Med, 1986. 10(5-6): p. 479-514.
- Diagnosis and initial management of nonmalignant diseases related to asbestos. Am J Respir Crit Care Med, 2004.170(6): p. 691-715.
- Churg, A., M.L. Warnock, and N. Green, Analysis of the cores of ferruginous (asbestos) bodies from the general population. II. True asbestos bodies and pseudoasbestos bodies. Lab Invest, 1979. 40(1): p. 31-8.
- Johnson, N.F., et al., Identification of inorganic dust particles in bronchoalveolar lavage macrophages by energy dispersive x-ray microanalysis. Arch Environ Health, 1986. 41(3): p. 133-44.
- Hammond, E.C., I.J. Selikoff, and H. Seidman, Asbestos exposure, cigarette smoking and death rates. Ann N Y Acad Sci, 1979. 330: p. 473-90.
- Zitting, A.J., et al., Radiographic small lung opacities and pleural abnormalities in relation to smoking, urbanization status, and occupational asbestos exposure in Finland. J Occup Environ Med, 1996. 38(6): p. 602-9.
- Churg, A. and B. Stevens, Enhanced retention of asbestos fibers in the airways of human smokers. Am J Respir Crit Care Med, 1995. 151(5): p. 1409-13.
- Lee, B.W., et al., Association of cigarette smoking and asbestos exposure with location and histology of lung cancer. Am J Respir Crit Care Med, 1998. 157(3 Pt 1): p. 748-55.
- Yazicioglu, S., et al., Pleural calcification, pleural mesotheliomas, and bronchial cancers caused by tremolite dust. Thorax, 1980. 35(8): p. 564-9.
- Baris, Y.I., et al., An outbreak of pleural mesothelioma and chronic fibrosing pleurisy in the village of Karain/Urgup in Anatolia. Thorax, 1978. 33(2): p. 181-92.