Reviewed By Allergy, Immunology & Inflammation Assembly
Submitted by
Aaron S. Bruns, M.D.
The Ohio State University
Columbus, OH
Ken Knox, M.D.
Indiana University
Indianapolis, IN
John Mastronarde, M.D.
The Ohio State University
Columbus, OH
Submit your comments to the author(s).
History
A 59-year old white woman presented to the clinic for evaluation of dyspnea and an abnormal chest computed tomography (CT). Three years ago, she was diagnosed with breast cancer. One of twenty-nine axillary lymph nodes were positive for tumor, which was estrogen receptor positive. She was treated with surgery, radiation, and chemotherapy that included doxirubicin, cyclophosphamide,paclitaxel, and gemcitabine. She was then given anastrozole. She was followed closely over the next two years and had no evidence of recurrence.
Before developing breast cancer, the patient was physically active, walking 3 to 4 miles daily. However, over the last two years she had increasing dyspnea on exertion and was able to walk only 1 mile. Just prior to the visit a chest radiograph revealed hilar and mediastinal lymphadenopathy. A chest CT confirmed bilateral hilar and mediastinal lymphadenopathy as well as perilymphatic nodules less than a centimeter in diameter throughout the lungs. In addition, a positron emission tomography (PET) scan revealed uptake in several mediastinal lymph nodes with a standard uptake value of 8. The patient denied any cough, weight loss, night sweats, fevers, or occupational or travel-related exposures. A repeat mammogram and breast ultrasound were both negative.
Physical Exam
Lab
FEV1 2.77 (81%)
FVC 2.29 (86%)
FEV1/FVC 80.1%
TLC 4.18 (81%)
DLCO 20.3 (91%)
Chest CT: Multiple nodules smaller than a centimeter in diameter were present in both lungs with a perilymphatic distribution. A right paratracheal lymph node measured 1.9 cm. There was a 1.3 cm right precarinal lymph node, a 1.4 cm left anterior mediastinal lymph node, and a 1.4 cm subcarinal lymph node as well. There was no pleural effusion or pneumothorax (Figures 1 and 2).
PET scan: Uptake in several mediastinal lymph nodes with a standard uptake value of 8 (Images not available).
Figures
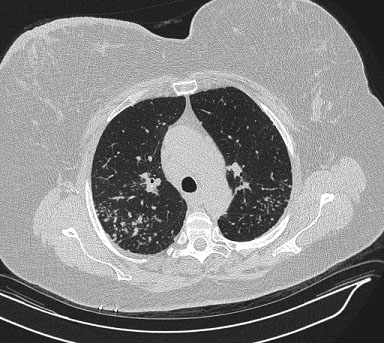
Figure 1. Axial view of high-resolution chest CT using lung windows showing multiple nodules less than one centimeter in diameter in a perilymphatic distribution.
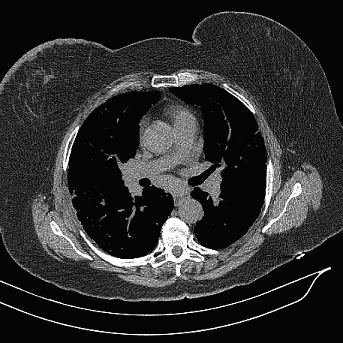
Figure 2. Axial view of high-resolution chest CT using mediastinal windows showing bilateral hilar and subcarinal lymphadenopathy.
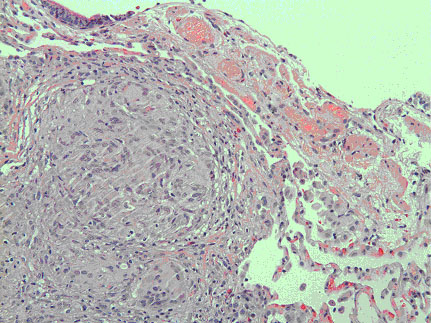
Figure 3. Slide of transbronchial biopsy showing multinucleated giant cells and epithelioid histiocytes in a granulomatous formation (Magnified 20x)
References
- Bergin C, Roggli V, Coblentz C et al. Secondary pulmonary lobule: normal and abnormal CT appearance. Am J Roentgenol 1988;151:21-25.
- Raoof S, Amchentsev A, Vlahos I et al. Pictorial Essay: Multinodular disease. A high-resolution CT scan diagnostic algorithm. Chest 2006;129:805-815.
- Gruden JF, Webb WR, Warnock M. Centrilobular opacities on HRCT: diagnosis and differential diagnosis with pathologic correlation. Am J Roentgenol 1994;162:569-574.
- Collins J, Blankenbaker D, Stern EJ. CT patterns of bronchiolar disease: what is tree-in-bud? Am J Roentgenol 1998;171:365-370.
- Brincker H, Wilbek E. The incidence of malignant tumors in patients with respiratory sarcoidosis. Br J Cancer 1974;29:247-251.
- Brincker H. Solid tumors preceding or following sarcoidosis. Med Pediatr Oncol 1987;15:82-88.
- Israel HL. Sarcoidosis, malignancy, and immunosuppressive therapy. Arch Int Med 1978;138:907-908.
- Askling J, Grunewald J, Eklund A et al. Increased risk for cancer following sarcoidosis. Am J Respir Crit Care Med 1999;160:1668-1672.
- Kurata A, Terado Y, Schulz A et al. Inflammatory cells in the formation of tumor-related sarcoid reactions. Hum Pathol 2005;36:546-554.
- Cohen PR, Kurzrock R. Sarcoidosis and malignancy. Clinics Derm 2007;25:326-333.
- Romer FK. Sarcoidosis and cancerâ€â€a critical view. Proceedings of the VIIIth International Conference on Sarcoidosis. Cardiff: Alpha Omega Press; 1980:567-571.
- Yu JQ, Zhuang H, Mavi A, Alavi A. Evaluating the role of flurodeoxyglucose PET imaging in the management of patients with sarcoidosis. PET Clin 2006;1:141-152.
- Hamper UM, Fishman EK, Khouri NF et al. Typical and atypical CT manifestations of pulmonary sarcoidosis. J Comput Assist Tomogr 1986;10:928-936.
- Alavi A, Gupta N, Alberini JL et al. Positron emission tomography imaging in nonmalignant thoracic disorders. Semin Nucl Med 2002;32:293-321.
- Yamada Y, Uchida Y, Tatsumi K et al. Fluorine-18-fluorodeoxyglucose and carbon-11-methionine evaluation of lymphadenopathy in sarcoidosis. J Nuc Med 1998;39:1160-1166.
- Lewis PJ, Salama A. Uptake of fluorine-18-fluorodeoxyglucose in sarcoidosis. J Nuc Med 1994;35:1647-1649.
- Cook GJ, Fogelman I, Maisey MN. Normal physiological and benign pathological variants of 18-fluro-2-deoxyglucose positron emission tomography scanning: potential for error in interpretation. Semin Nucl Med 1996;26:308-314.
- Kaira K, Oriuchi N, Otani Y et al. Diagnostic usefulness of fluorine-18-α-methyltyrosine positron emission tomography in combination with 18F-fluorodeoxyglucose in sarcoidosis patients. Chest 2007;131:1019-1027.
- Reich JM. Neoplasia in the etiology of sarcoidosis. Eur J Int Med 2006;17:81-87.
- O’Connell MJ, Schimpff SC, Krischner RH et al. Epithelioid granulmoas in Hodgkin’s disease. JAMA 1975;233:886-889.
- Yeager H Jr, Williams MC, Beekman JF et al. Sarcoidosis: analysis of cells obtained by bronchial lavage. Am Rev Respir Dis 1977;116:951-954.
- Winterbauer RH, Lammert J, Selland M et al. Bronchoalveolar lavage cell populations in the diagnosis of sarcoidosis. Chest 1993;104:352-361.
- American Thoracic Society. Statement on sarcoidosis. Am J Respir Crit Care Med 1999;160:736-755.
- Roethe RA, Fuller PB, Byrd RB et al. Transbronchoscopic lung biopsy in sarcoidosis. Optimal number and sites for diagnosis. Chest 1980;77:400-402.
- Trisolini R, Agli LL, Cancellieri A et al. The value of flexible transbronchial needle aspiration in the diagnosis of stage I sarcoidosis. Chest 2003;124:2126-2130.
- Garwood S, Judson MA, Silvestri G et al. Endobronchial ultrasound for the diagnosis of pulmonary sarcoidosis. Chest 2007;132:1298-1304.



