Reviewed By Clinical Problems Assembly
Submitted by
Jamie L. Garfield, MD
Fellow
Pulmonary and Critical Care Medicine
Temple University School of Medicine
Philadelphia, Pennsylvania
Victor Kim, MD
Assistant Professor of Medicine
Temple University School of Medicine
Philadelphia, Pennsylvania
Submit your comments to the author(s).
History
A 45-year-old white female presents to pulmonary clinic for evaluation of increasing chest tightness, cough and dyspnea. She has a history of chronic respiratory symptoms since childhood and frequent exacerbations of bronchitis, but no history of respiratory failure. She reports that until 1 year ago she was limited by mild pleuritic chest tightness and shortness of breath with heavy exertion. She now reports daily symptoms of fatigue, dyspnea, and exercise intolerance with minimal exertion. She has persistent dry cough and occasionally expectorates granular mucus. She has been using 3 liters per minute of supplemental oxygen via nasal cannula for the past year.
Her past medical history is significant for polycythemia, gastroesophageal reflux disease, fibronodular breast disease, chronic tinnitus with hearing loss and genital herpes. Her current medications include famotidine, diltiazem, valacyclovir, inhaled fluticasone, salmeterol and albuterol. She has a 30 pack-year smoking history, having quit smoking 5 years ago. She drinks 1-2 beers per week and she denies illicit drug use. She is a homemaker and reports no occupational exposures. Her parents, siblings and 2 children (ages 16 and 24) are alive and well with no respiratory disease or malignancy.
Physical Exam
Lab
White blood cell count 12,900/mm3, Hemoglobin 15.5 mg/dl, Platelet count 473,000/mm3.
BUN 9 mg/dl, creatinine 1.0 mg/dl, calcium 8.8 mg/dl and phosphate 4.9 mg/dl.
PT, PTT, electrolytes, glucose and liver function tests were within normal limits.
Arterial blood gas on 3L/min supplemental oxygen revealed a pH of 7.39, PCO2 40 mm Hg and PaO2 62 mm Hg.
Studies:
Echocardiogram: left ventricular ejection fraction was 55-65% and grade 1 diastolic dysfunction was noted; right ventricle was mildly dilated and had mildly depressed systolic function; pulmonary artery systolic pressure was estimated to be 48-52 mm Hg; right atrium was mildly dilated and there was mild tricuspid regurgitation.
Cardiac Catheterization: PAP: 30/6/13; PCWP: 2; CO: 3.38; CI: 2.16.
Pulmonary Function Tests: FEV1/ FVC: 74%; FEV1: 0.96 L, 39%; FVC: 1.29L, 42%; TLC: 2.27L, 53%; RV: 1.14L, 79%; DLCO: 3.11L, 57%.
6-Minute Walk Test: Resting SpO2: 86% RA; 92% on 2L/min; 8L/min was required to maintain oxygen saturation above 90% at the end of 6 minutes; the patient was able to walk 211 meters.
Figures
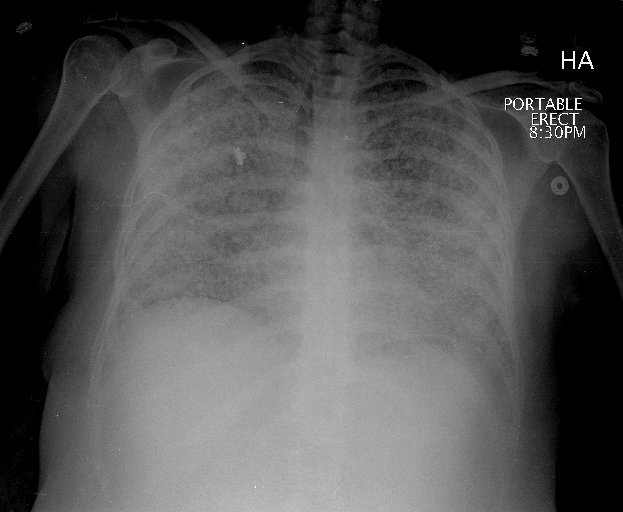
Figure 1: Posterior-anterior (PA) chest radiograph with extensive, poorly defined nodular opacities throughout both lungs and apical bullous disease.

Figure 2: Coronal view of high-resolution chest CT showing extensive bilateral parenchymal calcifications, focal areas of mild emphysematous changes predominantly in the upper lobes, and mild mediastinal and hilar adenopathy.

Figure 3: Bronchoalveolar lavage: Slightly mucoid, tan fluid; cultures revealed no growth; cytology showed no evidence of malignancy; a few white blood cells were noted, predominantly macrophages; laminated calcified concretions and debris were also present. Von Kossa stain positive.
References
- Castellana G, Gentile M, Castellana R, Fiorente P, Lamorgese V. Pulmonary alveolar microlithiasis: Clinical features, evolution of the phenotype, and review of the literature. Am J Med Genet 2002;111:220-224.
- Kliegman RM, Behrman RE, Jenson HB, Stanton BMD, Zitelli BJ, Davis HW. Nelson textbook of pediatrics, 18th ed. Philadelphia: WB Saunders; 2007.
- Volle E, Kaufmann HJ. Pulmonary alveolar microlithiasis in pediatric patients--review of the world literature and two new observations. Pediatr Radiol 1987;17:439-442.
- Gasparetto EL, Tazoniero P, Escuissato DL, Marchiori E, Frare E Silva RL, Sakamoto D. Pulmonary alveolar microlithiasis presenting with crazy-paving pattern on high resolution CT. Br J Radiol: 2004;77:974-976.
- Castellana G, Lamorgese V. Pulmonary alveolar microlithiasis: world cases and review of the literature. Respiration 2003;70:549-555.
- Deniz O, Ors F, Tozkoparan E, Ozcan A, Gumus S, Bozlar U, Bilgic H, Ekiz K, Demirci N. High resolution computed tomographic features of pulmonary alveolar microlithiasis. Eur J Radiol 2005;55:452-460.
- Prakash UB. Pulmonary alveolar microlithiasis. Semin Respir Crit Care Med 2002;23:103-113.
- Viswanathan R. Pulmonary alveolar microlithiasis. Thorax 1962;17:251-256.
- Prakash UB, Barham SS, Rosenow EC,3rd, Brown ML, Payne WS. Pulmonary alveolar microlithiasis. A review including ultrastructural and pulmonary function studies. Mayo Clin Proc 1983;58:290-300.
- Chinachoti N, Tangchai P. Pulmonary alveolar microlithiasis associated with the inhalation of snuff in thailand. Dis Chest 1957;32:687-689.
- Portnoy LM, Amadeo B, Hennigar GR. Pulmonary alveolar microlithiasis: an unusual case (associated with milk-alkali syndrome). Am J Clin Pathol 1964;41:194-201.
- Richardson J, Slovis B, Miller G, Dummer S. Development of pulmonary alveolar microlithiasis in a renal transplant recipient. Transplantation 1995;59:1056-1057.
- Pant K, Shah A, Mathur RK, Chhabra SK, Jain SK. Pulmonary alveolar microlithiasis with pleural calcification and nephrolithiasis. Chest 1990;98:245-246.
- Batchelor TJ, Ngaage DL, McGivern DV, Cowen ME. Surgical management of pneumothorax in pulmonary alveolar microlithiasis. Ann Thorac Surg 2007;84:290-292.
- Chan ED, Morales DV, Welsh CH, McDermott MT, Schwarz MI. Calcium deposition with or without bone formation in the lung. Am J Respir Crit Care Med 2002;165:1654-1669.
- Huqun, Izumi S, Miyazawa H, Ishii K, Uchiyama B, Ishida T, Tanaka S, Tazawa R, Fukuyama S, Tanaka T, Nagai Y, Yokote A, Takahashi H, Fukushima T, Kobayashi K, Chiba H, Nagata M, Sakamoto S, Nakata K, Takebayashi Y, Shimizu Y, Kaneko K, Shimizu M, Kanazawa M, Abe S, Inoue Y, Takenoshita S, Yoshimura K, Kudo K, Tachibana T, Nukiwa T, Hagiwara K. Mutations in the SLC34A2 gene are associated with pulmonary alveolar microlithiasis. Am J Respir Crit Care Med 2007;175:263-268.
- Hagiwara K. [Analysis of genes responsible for pathogenesis of pulmonary alveolar microlithiasis]. Nippon Naika Gakkai Zasshi 2006; 95:1036-1041.
- Gocmen A, Toppare MF, Kiper N, Buyukpamukcu N. Treatment of pulmonary alveolar microlithiasis with a diphosphonate--preliminary results of a case. Respiration 1992;59:250-252.
- Edelman JD, Bavaria J, Kaiser LR, Litzky LA, Palevsky HI, Kotloff RM. Bilateral sequential lung transplantation for pulmonary alveolar microlithiasis. Chest 1997;112:1140-1144.
- Moon E, Tsuang W, Bonnette P, Jackson K, Lien D, Blumenthal N, Kotloff R, Ahya V. Lung transplantation outcomes for pulmonary alveolar microlithiasis: A limited case series. Am J Respir Crit Care Med 2009;179:A4602 [abstract].
- Tachibana T, Hagiwara K, Johkoh T. Pulmonary alveolar microlithiasis: Review and management. Curr Opin Pulm Med 2009;15:486-490.



