The diagnosis that best explains our patient’s presentation is myasthenic syndrome with crisis, resulting from impairment of signal transmission at the neuromuscular junction. The other options listed describe myotonic dystrophy (B), multiple sclerosis (C), and amyotrophic lateral sclerosis (D), which typically present with progressive worsening of symptoms over a prolonged period of time, and are unlikely to have an initial presentation of acute respiratory failure, as was the case here. It is important to remember that in the setting of myasthenic syndrome the differential is broad and includes myasthenia gravis, Guillain-Barré, Lambert-Eaton Myasthenic Syndrome, certain medications, organophosphate poisoning, tick paralysis, and botulism (1, 2). Based on our patient’s history and clinical presentation, myasthenia gravis is the most likely diagnosis
Myasthenic crisis is defined as either respiratory failure requiring invasive mechanical ventilation, or a delay in postoperative extubation of more than twenty-four hours because of inadequate ventilation attributed to weakened respiratory muscles, airway collapse due to bulbar weakness, or inability to clear secretions. Patients at risk for crisis should be closely observed as their pattern of muscle weakening begins with the intercostals and accessory muscles followed by the diaphragm, masking the early, overt signs of respiratory distress, as was seen in our patient. Approximately 20% of all patients with myasthenia will develop crisis at some point, with an associated mortality rate that has declined over the last few decades from 75% to less than 5% (1-4).
There is no air-fluid level seen on either view to support the diagnosis of pleural effusion, and the lateral view clearly demonstrates a mass-like lesion, the epicenter of which lies in the anterior mediastinum. Developing a differential for a mediastinal mass requires understanding its boundaries and divisions. The boundaries of the mediastinum itself are the thoracic inlet, the diaphragm, and the pleural sacs. The anterior division of the mediastinum extends from the sternum to the pericardium and brachiocephalic vessels, the posterior division extends from the pericardium and trachea to the vertebral column, and the middle division fills the space between the anterior and posterior mediastinum (Table 1)(5). This patient presented with an anterior mediastinal mass, the most common of which are thymomas, teratomas, thyroid malignancies, and lymphomas. Of these, thymoma has the highest incidence, representing 50% of all anterior mediastinal neoplasms in adults. Thymomas most often develop between the ages of 40-60 and only a third of patients will develop symptoms directly related to the tumor’s effects on surrounding structures. As a result, the diagnosis is often made as an incidental finding on a chest radiograph obtained for other causes. Most thymomas are indolent tumors, which may appear solid, cystic, or hemorrhagic on computed tomography, and up to 50% of thymomas will demonstrate some sort of paraneoplastic syndrome. Distant metastases are uncommon (<7%); however, local invasion can occur up to 32% of the time (5-8).
In addition to the fact that thymomas have the highest incidence among masses of the anterior mediastinum, the presence of myasthenic symptoms increases the suspicion for thymoma in this patient. The prevalence of myasthenia gravis is approximately 10 per 100,000, and the presence of a thymoma significantly increases the likelihood of this disorder. While only 15% of patients with myasthenia gravis have thymomas, around 30% of patients with thymoma have myasthenia, making it the most common paraneoplastic syndrome associated with this neoplasm (3, 6, 9). This is a true paraneoplastic syndrome caused by the presence of an epitope on thymoma cells that is also found on the acetylcholine receptors at the neuromuscular junction. As the immune system responds to the presence of the thymoma, antibodies interacting with both the thymoma and the neuromuscular junction are generated in the thymus, resulting in myasthenia. Our patient’s thymoma along with his clinical symptoms of bulbar, respiratory, and ocular muscle weakness, without significant limb involvement, is typical of paraneoplastic myasthenia gravis (8-10).
|
Table 1: Differential of Mediastinal Masses
|
|
Anterior
|
Middle
|
Posterior
|
|
Thymomas
|
Lymphadenopathy resulting from metastatic disease
|
Neurogenic tumors
|
|
Lymphomas
|
Vascular masses
|
Meningoceles
|
|
Teratomatous neoplasms
|
Granulomatous disease
|
Gastroenteric cysts
|
|
Thyroid masses
|
Pericardial cyst
|
Diaphragmatic hernias
|
|
Aortic aneurysm
|
Bronchogenic cyst
|
Esophageal diverticula
|
Our patient underwent CT scanning to better characterize the lesion (Figure 2). A transthoracic fine needle aspirate was performed, which was found to be consistent with the diagnosis of thymoma.

Figure 2: Axial CT image showing right atrial collapse and stretching of the right pulmonary vein.
Given the clinical suspicion of myasthenia gravis, imaging of the brain and spinal cord is not likely to provide helpful information, as there are no specific findings that correlate with the diagnoses listed in our differential. Given the strong suspicion for myasthenic crisis in this patient, the simplest place to start is to check for the presence of serum antibodies to acetylcholine receptors (ACh-R) and muscle specific tyrosine kinase (MuSK). ACh-R antibodies are found in 90% of patients with generalized myasthenia, 50% of patients with ocular myasthenia, and a positive titer is 100% specific for the diagnosis of myasthenia gravis. In patients with generalized myasthenia who do not have ACh-R antibodies, approximately 70% will have MuSK antibodies, however MuSK antibodies are never positive in either thymomatous myasthenia gravis or in patients who test positive for ACh-R antibodies (4, 10).
Electrodiagnostic studies, including electromyography and nerve conduction studies can be helpful as they provide a way to screen for multiple causes of muscle weakness simultaneously. Both nerve conduction studies and electromyography show decreasing motor response to repetitive nerve stimulation in myasthenia and have sensitivities of 80 percent and greater than 90 percent respectively. Other tests to consider are edrophonium testing (tensilon test) and either computed tomography or magnetic resonance imaging of the thorax to evaluate for thymoma, if not already done(4).
Our patient had both ACh-R and MuSK antibody levels drawn on admission. The ACh-R antibody level was greater than 10 times the upper limit of normal and MuSK antibodies were not detected.
In nearly every case of myasthenic crisis, a review of recent events will reveal a known risk factor. There are numerous potential causes, with one series showing respiratory infection to be the most common cause at 29% (2). Myasthenic crisis occurs most frequently within a year of the onset of myasthenic symptoms, and in patients with paraneoplastic myasthenia due to a thymoma, it may be the presenting symptom. Commonly prescribed medications are another frequent cause of crisis (Table 2). Interestingly, initiation of corticosteroids, which are frequently used in treatment of myasthenia, can precipitate crisis during the first week of treatment due to transient muscle weakening. Those patients having the highest risk of crisis with initiation of steroids are individuals having bulbar symptoms. Other causes of myasthenic crisis include: sepsis, aspiration pneumonitis, emotional stress, and iodinated contrast agents. Pregnancy is also a significant risk factor with 33% of pregnant patients with myasthenia gravis developing crisis, which is associated with high perinatal mortality. It should be noted that edrophonium testing should be avoided in patients identified to be at risk for crisis as it can increase respiratory secretions and lead to the onset of crisis (1-4).
|
Table 2: Medications which can exacerbateMyasthenia
|
|
Antibiotics
|
Aminoglycosides
Quinolones
Macrolides
Antimalarials
|
|
Cardiovascular drugs
|
Quinidine
Procainamide
Beta blockers
Calcium channel blockers
|
|
Neuromuscular junction blockers
|
Succinylcholine
Vecuronium
|
|
Anticonvulsants
Magnesium salts
|
Phenytoin, carbamazepine
|
|
Corticosteroids
Long-acting benzodiazepines
|
|
High dose corticosteroids and either plasmapheresis or IVIG are essential in the management of patients with myasthenic crisis. In patients found to have a thymoma, surgery should be delayed only until the patient has undergone a complete course of plasmapheresis or IVIG for symptom stabilization as thymectomy may prevent a prolonged episode of crisis. Although muscle weakness can occur with the initiation of corticosteroids, this risk is minimized by the simultaneous administration of IVIG and plasmapheresis, and steroids will actually shorten the time to recovery of muscle strength. The decision on whether to use plasmapheresis or IVIG depends on the availability of plasmapheresis at a given institution and the presence of contraindications in a given patient, as studies have not consistently demonstrated an advantage of one over the other. Plasmapheresis results in decreased levels of circulating antibodies and complement, and is usually performed five times, with exchanges occurring every other day. Patients treated with plasmapheresis typically show improvement within three days of initiation of therapy and the response generally lasts for several weeks. Complications associated with plasmapheresis are most often associated with the insertion and maintenance of the line required for exchanges and with the large volume shifts occurring with each exchange. Because of the volume shifts, plasmapheresis is not an appropriate therapy for certain groups of patients such as those who are pregnant, septic, hypotensive, or those with heart failure. IVIG is associated with a less predictable response and longer time to improvement of symptoms, which can be up to nineteen days, but generally has fewer adverse events when compared with plasmapheresis. The most serious adverse event associated with IVIG is anaphylaxis, which can occur if IVIG is given to IgA deficient individuals. Other adverse reactions include serum sickness, headache, chills, renal failure, and myalgias(1-5, 11).
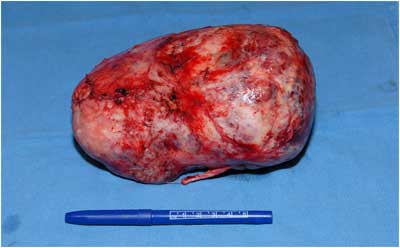
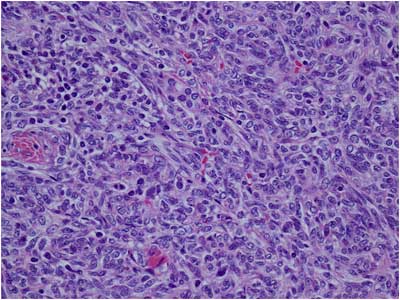
Our patient received high-dose corticosteroids and five rounds of plasmapheresis without complication before going to the operating room for thymectomy. The tumor was successfully resected (Figure 3) and found to be non-invasive on both macroscopic and microscopic examination. The final pathology report showed the tumor to be World Health Organization (WHO) Type A with spindled/ovoid morphology (Figure 4). His post-operative course was uneventful and he was discharged to home two weeks after surgery.
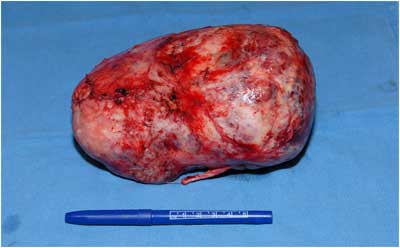
Figure 3: The excised thymoma, measuring 16.5 x 15.5 x 8.4 cm.
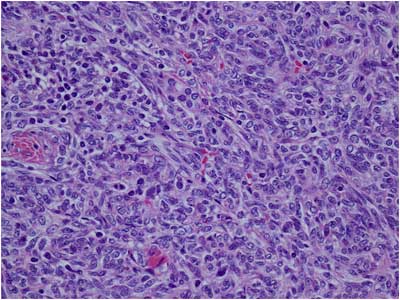
Figure 4: Surgical pathology image demonstrating thymoma with WHO Type A morphology.
While our patient’s overall prognosis is good, the likelihood of post-operative remission of paraneoplastic myasthenia gravis is low. Only about 16% of patients with paraneoplastic myasthenia experience complete remission after surgery, and there is increased risk for non-remission associated with tumor size greater than 6cm (8, 12, 13). Both WHO type and Masaoka Stage of the tumor correlate well with predicted long-term survival. In our patient with a WHO Type A and Masaoka Stage 1 tumor, his 5-year survival is between 96-100%. Once the thymoma is removed, the general course of patient with paraneoplastic myasthenia is no different from any other myasthenic patient, and the likelihood of recurrence of crisis is low except in those with late-onset disease (1, 5, 8)
|
Table 3: Masaoka Staging System
|
|
Stage
|
Invasiveness
|
5 year Survival
|
|
1
|
Macroscopic: tumor is completely encapsulated
Microscopic: no evidence of capsular invasion
|
96-100%
|
|
2
|
Macroscopic: tumor has spread beyond capsule into the mediastinal pleura or adipose
Microscopic: evidence of capsular invasion
|
86-95%
|
|
3
|
Macroscopic: invasion into nearby organs
|
56-69%
|
|
4a
|
Macroscopic: spread through pleural or pericardial space
|
11-50%
|
|
4b
|
Metastasis via lymphatic or hematogenous routes
|
Acknowledgements: The authors would like to thank Drs. Tyson Neumann, David Hormuth, Ashley Inman, and Daryl Heitkamp for their assistance in gathering the clinical information for this case.