Reviewed By Critical Care Assembly
Submitted by
Timothy R. Watkins, MD
Acting Instructor of Medicine
Division of Pulmonary and Critical Care Medicine
University of Washington, Harborview Medical Center
Seattle, WA
Colin R. Cooke, MD, MSc
Senior Fellow
Division of Pulmonary and Critical Care Medicine
University of Washington, Harborview Medical Center
Seattle, WA
Submit your comments to the author(s).
History
A 67-year-old man who was recently diagnosed with pulmonary tuberculosis and treated with four-drug antituberculous directly observed therapy for the last month presented to the emergency department with hemoptysis. The patient stated he had small amounts of blood-streaked sputum for the past 2 weeks, but noted that immediately prior to coming to the emergency department he had coughed up approximately “a cup” of bright red blood. While still in the emergency department, he had a witnessed episode of large volume hemoptysis, estimated to be greater than 250 cc of fresh blood.
The patient’s past medical history was unremarkable with the exception of longstanding tobacco abuse. Other than his recent antituberculous therapy he took no regular medications. He did not regularly use aspirin or other NSAIDs. He had no history of rash, kidney disease, hematuria, or known autoimmune disease. Prior to the episodes described above, he had no history of pneumonia or hemoptysis.
The patient smoked one pack of cigarettes per day for the past 45 years. He did not use alcohol or other recreational drugs. He emigrated from Ethiopia to the United States 10 years earlier. The patient was single, living with his brother’s family. He worked as a carpenter until 2 to 3 months earlier when he became ill.
Physical Exam
Lab
Hematocrit 12%
Platelet count was 378,000/mm3
BUN 49 mg/dl, serum creatinine was 1.1 mg/dl
Alkaline phosphatase 124mg/dl
Total bilirubin 1.4mg/dl
AST 50 IU/L, ALT 29 IU/L
The patient’s electrolytes and serum glucose were within normal limits.
An INR and PTT were within normal limits.
A urinalysis showed an elevated specific gravity and the presence of hyaline casts.
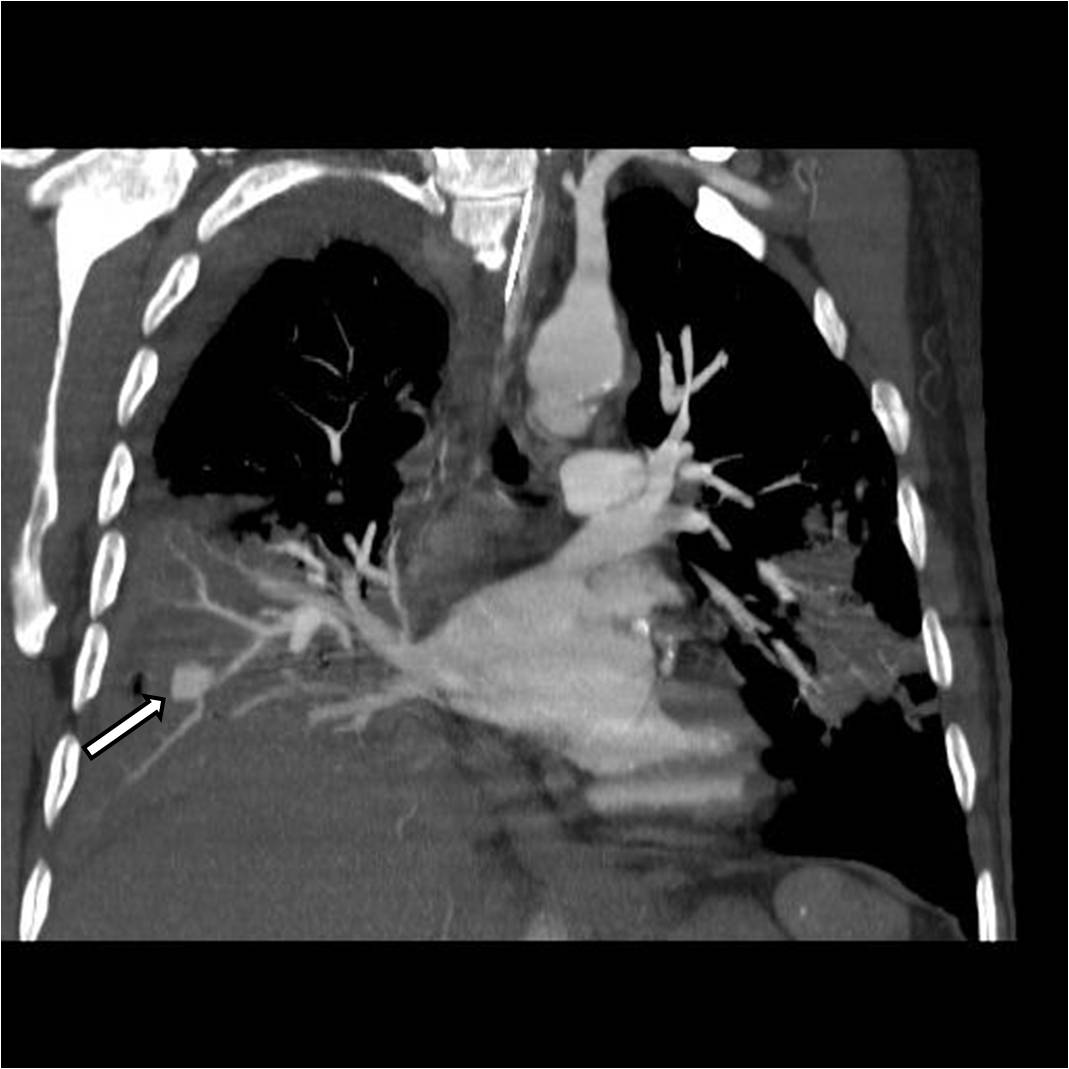
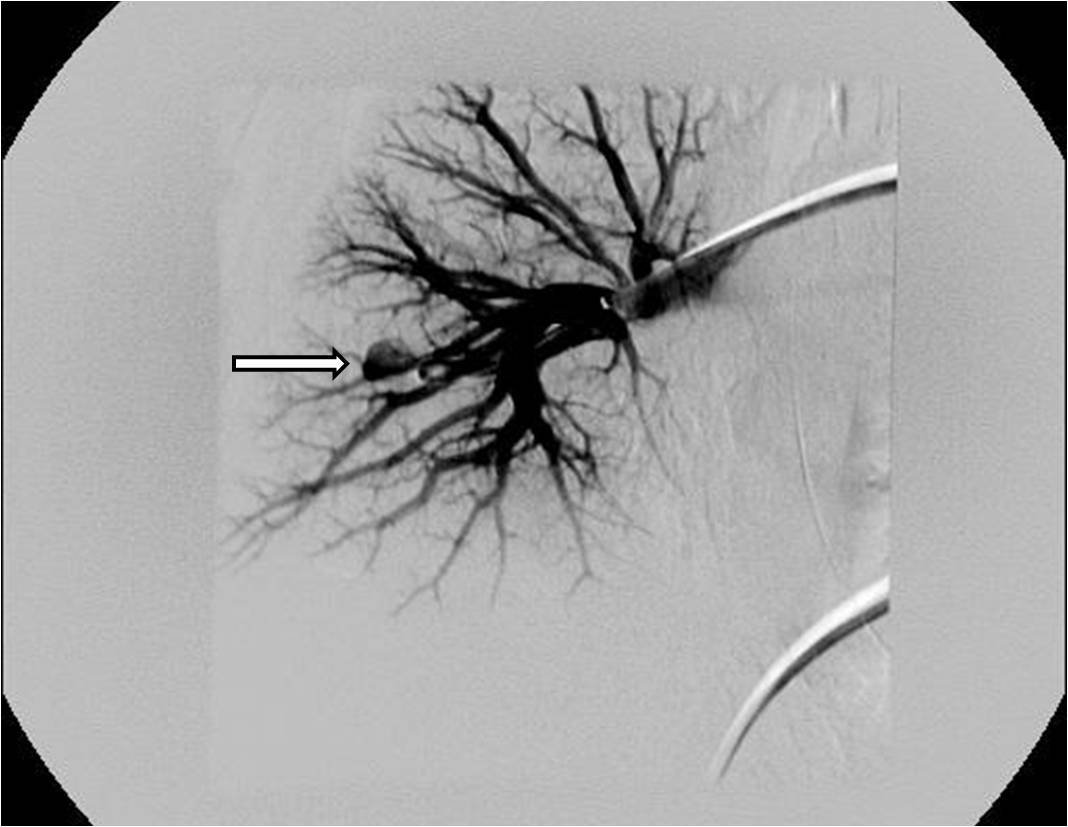
Figures
References
- Conlan AA, Hurwitz SS, Krige L, Nicolaou N, Pool R. Massive hemoptysis. Review of 123 cases. J Thorac Cardiovasc Surg 1983;85:120-124.
- Jean-Baptiste E. Clinical assessment and management of massive hemoptysis. Crit Care Med 2000;28:1642-1647.
- Strange C. Double-lumen endotracheal tubes. Clin Chest Med 1991;12:497-506.
- Klein U, Karzai W, Bloos F, et al. Role of fiberoptic bronchoscopy in conjunction with the use of double-lumen tubes for thoracic anesthesia: a prospective study. Anesthesiology 1998;88:346-350.
- Haponik EF, Chin R. Hemoptysis: clinicians' perspectives. Chest 1990;97:469-75.
- Cahill BC, Ingbar DH. Massive hemoptysis. Assessment and management. Clin Chest Med 1994;15:147-167.
- Dye C, Scheele S, Dolin P, et al. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA 1999;282:677-686.
- Knott-Craig CJ, Oostuizen JG, Rossouw G, et al. Management and prognosis of massive hemoptysis. Recent experience with 120 patients. J Thorac Cardiovasc Surg 1993;105:394-397.
- Daoud MS, Gibson LE, DeRemee RA, et al. Cutaneous Wegener's granulomatosis: clinical, histopathologic, and immunopathologic features of thirty patients. J Am Acad Dermatol 1994;31:605-612.
- Hoffman GS, Kerr GS, Leavitt RY, et al. Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 1992;116:488-498.
- Johnston H, Reisz G. Changing spectrum of hemoptysis. Underlying causes in 148 patients undergoing diagnostic flexible fiberoptic bronchoscopy. Arch Intern Med 1989;149:1666-1668.
- Santiago S, Tobias J, Williams AJ. A reappraisal of the causes of hemoptysis. Arch Intern Med 1991;151:2449-2451.
- Reisz G, Stevens D, Boutwell C, Nair V. The causes of hemoptysis revisited. A review of the etiologies of hemoptysis between 1986 and 1995. Mo Med 1997;94:633-635.
- McGuinness G, Beacher JR, Harkin TJ, et al. Hemoptysis: prospective high-resolution CT/bronchoscopic correlation. Chest 1994;105:1155-1162.
- Hirshberg B, Biran I, Glazer M, Kramer MR. Hemoptysis: etiology, evaluation, and outcome in a tertiary referral hospital. Chest 1997;112:440-444.
- Rasmussen V. On haemoptysis, especially when fatal, in its anatomical and clinical aspects. Edinburgh Med J 1968;14.
- Ungaro R, Saab S, Almond CH, Kumar S. Solitary peripheral pulmonary artery aneurysms. Pathogenesis and surgical treatment. J Thorac Cardiovasc Surg 1976;71:566-571.
- Erdogan A, Yegin A, Gurses G, Demircan A. Surgical management of tuberculosis-related hemoptysis. Ann Thorac Surg 2005;79:299-302.
- Metin M, Turna A, Sayar A, Gurses A. Prompt surgery for massive hemoptysis: more acceptable than it was reported. Eur J Cardiothorac Surg 2003;23:647.
- Poyanli A, Acunas B, Rozanes I, et al. Endovascular therapy in the management of moderate and massive haemoptysis. Br J Radiol 2007;80:331-336.
- Remy-Jardin M, Bouaziz N, Dumont P, et al. Bronchial and nonbronchial systemic arteries at multi-detector row CT angiography: comparison with conventional angiography. Radiology 2004;233:741-749.
- Swanson KL, Johnson CM, Prakash UB, et al. Bronchial artery embolization : experience with 54 patients. Chest 2002;121:789-795.
- Katoh O, Kishikawa T, Yamada H, et al. Recurrent bleeding after arterial embolization in patients with hemoptysis. Chest 1990;97:541-546.
- White RI, Jr. Bronchial artery embolotherapy for control of acute hemoptysis: analysis of outcome. Chest 1999;115:912-915.
- Mossi F, Maroldi R, Battaglia G, et al. Indicators predictive of success of embolisation: analysis of 88 patients with haemoptysis. Radiol Med 2003;105:48-55.
- Hayakawa K, Tanaka F, Torizuka T, et al. Bronchial artery embolization for hemoptysis: immediate and long-term results. Cardiovasc Intervent Radiol 1992;15:154-8; discussion 8-9.
- Wong ML, Szkup P, Hopley MJ. Percutaneous embolotherapy for life-threatening hemoptysis. Chest 2002;121:95-102.