Reviewed By Behavioral Science Assembly
Submitted by
Lokesh Venkateshaiah, MD
Fellow
Division of Pulmonary, Critical Care and Sleep Medicine
The MetroHealth System, Case Western Reserve University
Cleveland, Ohio
Bruce Arthur, MD
Fellow
Division of Pulmonary, Critical Care and Sleep Medicine
The MetroHealth System, Case Western Reserve University
Cleveland, Ohio
J. Daryl Thornton, MD, MPH
Assistant Professor
Division of Pulmonary, Critical Care and Sleep Medicine, Center for Reducing Health Disparities
The MetroHealth System, Case Western Reserve University
Cleveland, Ohio
Submit your comments to the author(s).
History
A 60-year-old man presented to the emergency department complaining of persistent right-sided chest pain and cough. The chest pain was pleuritic in nature and had been present for the last month. The associated cough was productive of yellow sputum without hemoptysis. He had unintentionally lost approximately 30 pounds over the last 6 months and had nightly sweats. He had denied fevers, chills, myalgias or vomiting. He also denied sick contacts or a recent travel history. He recalled childhood exposures to persons afflicted with tuberculosis.
The patient smoked one pack of cigarettes daily for the past 50 years and denied recreational drug use. He reported ingesting twelve beers daily and had had delirium tremens, remote right-sided rib fractures and a wrist fracture as a result of alcohol consumption. He had worked in the steel mills but had discontinued a few years previously. He collected coins and cleaned them with mercury.
The patient’s past medical history was remarkable for chronic “shakes” of the upper extremities for which he had not sought medical attention. Other than daily multivitamin tablets, he took no regular medications.
Hospital course
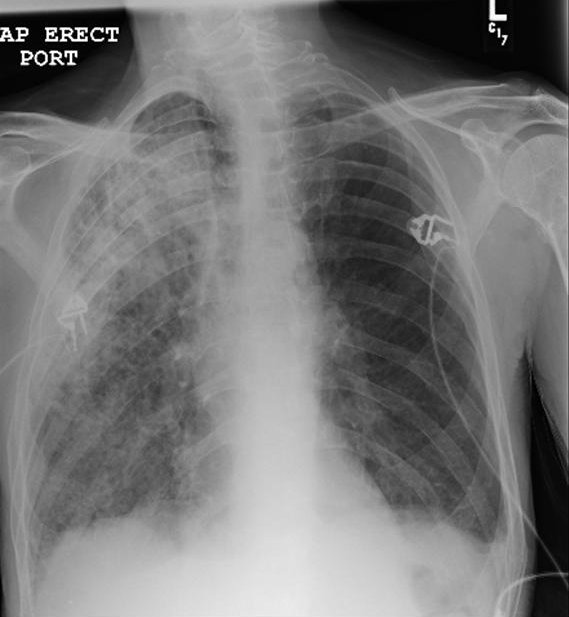
He was initially admitted to the general medical floor for treatment of community-acquired pneumonia (see Figure 1) and for the prevention of delirium tremens. He was initiated on ceftriaxone, azithromycin, thiamine and folic acid. Diazepam was initiated and titrated using the Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWAS-Ar), a measure of withdrawal severity (1). By hospital day 5, his respiratory status continued to worsen, requiring transfer to the intensive care unit (ICU) for hypoxemic respiratory failure. His neurologic status had also significantly deteriorated with worsening confusion, memory loss, drowsiness, visual hallucinations (patient started seeing worms) and worsening upper extremity tremors without generalized tremulousness despite receiving increased doses of benzodiazepines.
Physical Exam
Lab
White blood cell count was 11,000/mm3 with 38% neutrophils, 8% lymphocytes, 18 % monocytes and 35% bands
Hematocrit 33%
Platelet count was 187,000/mm3
Serum sodium was 125 mmol/L, potassium 3 mmol/L, chloride 91 mmol/L, bicarbonate 21 mmol/L, blood urea nitrogen 14 mg /dl, serum creatinine 0.6 mg/dl and anion gap of 14.
Urine sodium <10 mmol/L, urine osmolality 630 mosm/kg
Liver function tests revealed albumin 2.1 with total protein 4.6, normal total bilirubin, aspartate transaminase (AST) 49, Alanine transaminase (ALT) 19 and alkaline phosphatase 47.
Three sputum samples were negative for acid-fast bacilli (AFB).
Bronchoalveolar lavage (BAL) white blood cell count 28 cells/µl, red blood cell count 51 cells/µl, negative for AFB and negative Legionella culture. BAL gram stain was without organisms or polymorphonuclear leukocytes.
Blood cultures were negative for growth.
Sputum cultures showed moderate growth of Pasteurella multocida.
2D transthoracic ECHO of the heart showed normal valves and an ejection fraction of 65% with a normal left ventricular end-diastolic pressure and normal left atrial size. No vegetations were noted.
Purified protein derivative (PPD) administered via Mantoux testing was 8 mm in size at 72 hr after placement.
Human immunodeficiency virus (HIV) serology was negative.
Arterial blood gas (ABG) analysis performed on room air on presentation to the ICU: pH 7.49, PaCO2 29 mm Hg, PaO2 49 mm Hg.
Figures
References
- Sullivan JT, Sykora K, Schneiderman J, et al. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict 1989;84:1353-1357.
- Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:818-824.
- The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-1308.
- Agarwal R, Reddy C, Aggarwal AN, et al. Is there a role for noninvasive ventilation in acute respiratory distress syndrome? A meta-analysis. Respir Med 2006;100:2235-2238.
- Soyka M. Prevalence of alcohol-induced psychotic disorders. Eur Arch Psychiatry Clin Neurosci 2008;258:317-318.
- Tavel ME, Davidson W, Batterton TD. A critical analysis of mortality associated with delirium tremens. Review of 39 fatalities in a 9-year period. Am J Med Sci 1961;242:18-29.
- McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc 2003;51:591-598.
- Bateman T. Notes of a case of mercurial erethism. Medico-Chirurgical Transactions 1818;9:220-233.
- Buckell M, Hunter D, Milton R, et al. Chronic mercury poisoning. 1946. Br J Ind Med 1993;50:97-106.
- Rowens B, Guerrero-Betancourt D, et al. Respiratory failure and death following acute inhalation of mercury vapor. A clinical and histologic perspective. Chest 1991;99:185-190.
- Aguado S, de Quiros IF, Marin R, et al. Acute mercury vapour intoxication: report of six cases. Nephrol Dial Transplant 1989;4:133-136.
- Ibrahim D, Froberg B, Wolf A, et al. Heavy metal poisoning: clinical presentations and pathophysiology. Clin Lab Med 2006;26:67-97, viii.
- A fact sheet for health professionals - elemental mercury. Available from: http://www.idph.state.il.us/envhealth/factsheets/mercuryhlthprof.htm
- Clarkson TW, Magos L, Myers GJ. The toxicology of mercury - current exposures and clinical manifestations. N Engl J Med 2003;349:1731-1737.
- Boyd AS, Seger D, Vannucci S, et al. Mercury exposure and cutaneous disease. J Am Acad Dermatol 2000;43:81-90.
- Dargan PI, Giles LJ, Wallace CI, et al. Case report: severe mercuric sulphate poisoning treated with 2,3-dimercaptopropane-1-sulphonate and haemodiafiltration. Crit Care 2003;7:R1-6.
- Eto K. Minamata disease. Neuropathology 2000;20:S14-9.
- Bakir F, Damluji SF, Amin-Zaki L, et al. Methylmercury poisoning in Iraq. Science 1973;181:230-241.
- Berlin M, Carlson J, Norseth T. Dose-dependence of methylmercury metabolism. A study of distribution: biotransformation and excretion in the squirrel monkey. Arch Environ Health 1975;30:307-313.
- Harada M. Congenital Minamata disease: intrauterine methylmercury poisoning. Teratology 1978;18:285-288.
- Graeme KA, Pollack CVJ. Heavy metal toxicity Part I: Arsenic and mercury. J Emerg Med 1998;16:45-56.
- Aaseth J, Frieheim EA. Treatment of methylmercury poisoning in mice with 2,3-dimercaptosuccinic acid and other complexing thiols. Acta Pharmacol Toxicol (Copenh) 1978;42:248-252.
- Archbold GP, McGuckin RM, Campbell NA. Dimercaptosuccinic acid loading test for assessing mercury burden in healthy individuals. Ann Clin Biochem 2004;41:233-236.
- Kosnett MJ. Unanswered questions in metal chelation. J Toxicol Clin Toxicol 1992;30:529-547.
- Zimmer LJ, Carter DE. The efficacy of 2,3-dimercaptopropanol and D-penicillamine on methyl mercury induced neurological signs and weight loss. Life Sci 1978;23:1025-1034.