Reviewed By Clinical Problems Assembly
Submitted by
Misbah Baqir, MD
Senior Fellow
Mayo Clinic
Rochester, MN
Alvaro Velasquez, MD
Staff Physician
Divison of Pulmonary, Allergy and Critical Care Medicine
Emory University School of Medicine
Atlanta, GA
Octavian C. Ioachimescu, MD, PhD
Staff Physician
Division of Pulmonary, Allergy and Critical Care Medicine
Emory University School of Medicine, Atlanta VA Medical Center
Atlanta, GA
Submit your comments to the author(s).
History
A 38 year-old transsexual male presented to the emergency department with a three-day history of progressive dyspnea associated with a mild, non-productive cough. He also complained of a pleuritic-type chest pain and of dyspnea while speaking in longer sentences. He admitted feeling "hot and cold" at times, with no objective measurements of body temperature. Along with these symptoms he also reported lethargy. He denied wheezing, hemoptysis, sore throat, rash, significant weight changes, sick contacts or any recent travel.
Past medical history: the patient reported getting hormonal "shots" since age 16.
Past surgical history: none.
Medications at home: hormonal "shots"
Social History: denied smoking cigarettes, alcohol or illicit drugs.
Personal History: works as a hair stylist.
Family History: diabetes mellitus (mother)
Physical Exam
(Upon arrival to the emergency room)
The patient was alert and oriented. Pulse was 110 beats per minute, blood pressure 100/73 mm Hg, respiratory rate 30 per minute, temperature 37.8 ºC, Oxygen saturation was 90% on room air. No cyanosis or clubbing was noted. Pupils were equal and reactive to light. Neck examination revealed no abnormality. Precordial examination revealed tachycardia, but no murmurs, rubs or gallops. Patient demonstrated a rapid, shallow breathing pattern, but was not using accessory respiratory muscles. On auscultation he had normal vesicular breath sounds bilaterally. Abdomen was soft, with normal bowel sounds. Skin examination revealed several pinpoint, needle-like marks on the chest, buttocks and thighs. No peripheral edema was noted. His joints were non-tender, not warm to touch and free of swelling or deformity. Neurologic examination was within normal limits.
MORE INFORMATION:
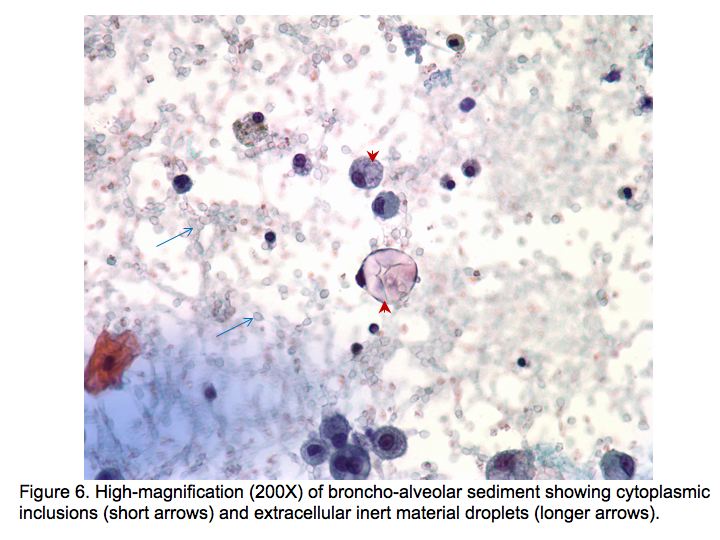
Upon further questioning triggered by the observed skin needle marks, the patient attributed them to hormonal injections and multiple subcutaneous inoculations with a substance which on the vial had no name, but the following chemical structure: Si(CH3)3-[C(CH3)2-Si-O]n-Si(CH3)3 .
Lab
Hemoglobin 8.8 g/dL, hematocrit 26.5%, WBCs 10,000 /mm3, Platelets 181,000/mm3, MCV 106 fL.
Differential: 77% segmented neutrophils, 12% lymphocytes, 3% eosinophils and 3% monocytes.
Creatinine 0.7 mg/dL, AST 47 U/L, ALT 40 U/L, alkaline phosphatase 40 U/L. PT, PTT and INR were normal. The patient’s electrolytes and serum glucose were within normal limits.
Figures
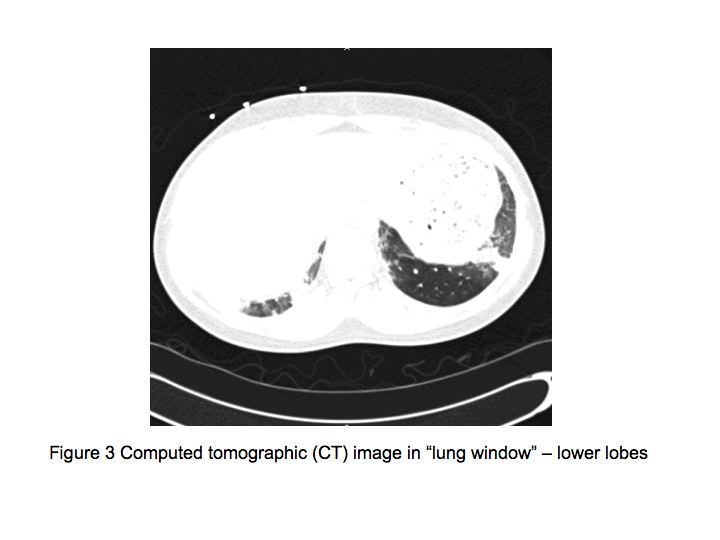
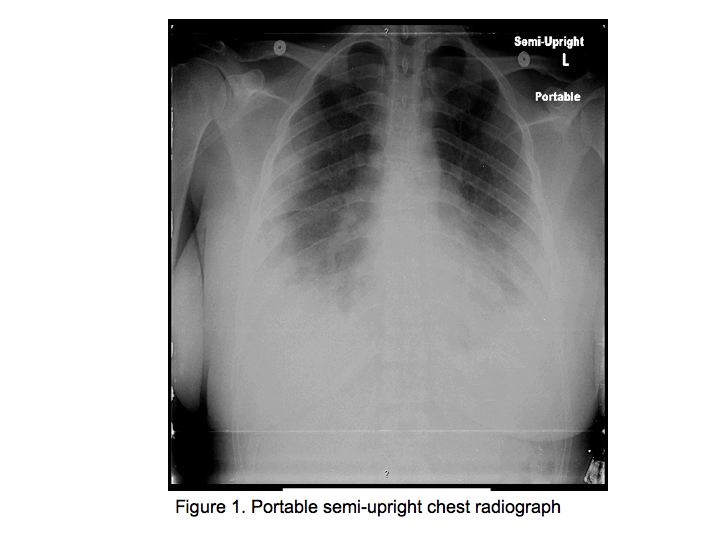
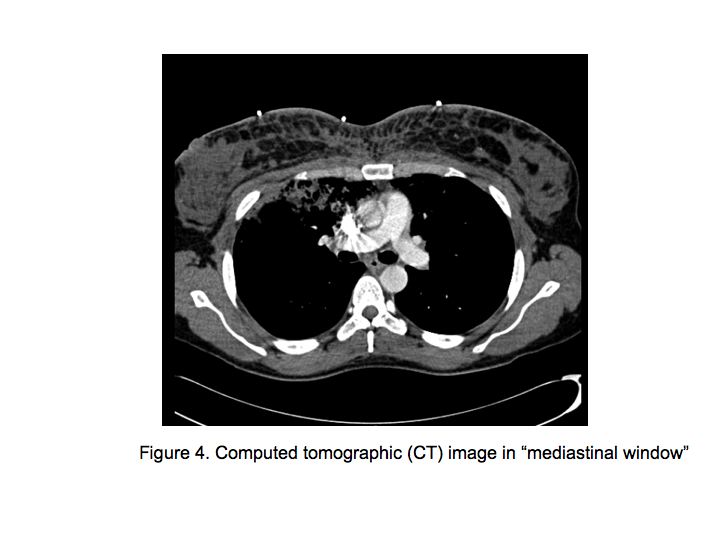
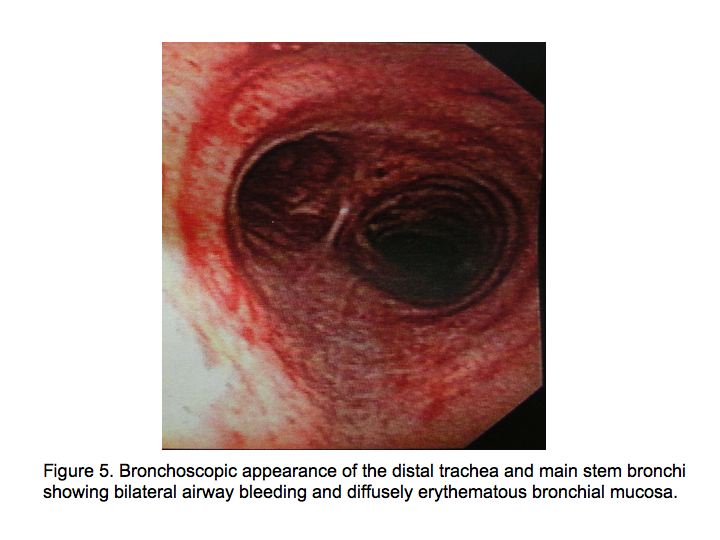
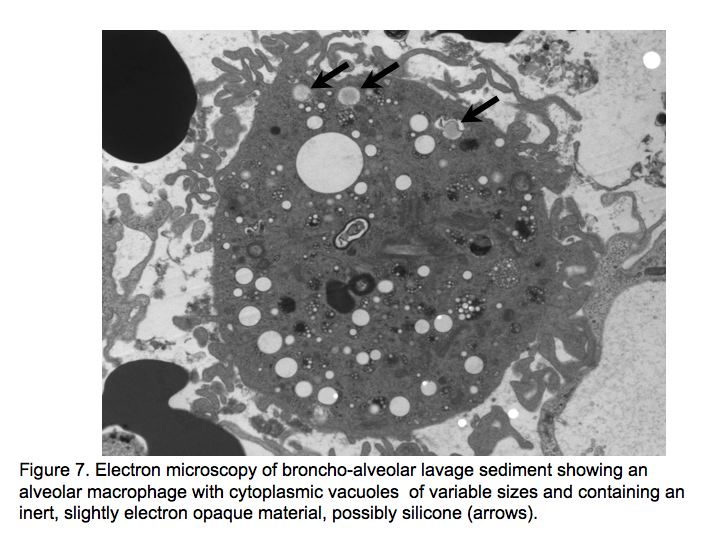
The patient was admitted to the medical floor and was started empirically on antibiotics. Cultures were obtained and an HIV test was done. Bronchoscopy was planned the next day which revealed diffuse erythema and hemorrhage in both the bronchial trees as shown in Fig. 5.
References
- Anastassov GE, Schulhof S, Lumerman H. Complications after facial contour augmentation with injectable silicone. Diagnosis and treatment. Report of a severe case. Int J Oral Maxillofac Surg. 2008; 37(10): 955-60.
- Ellenbogen R, Ellenbogen R, Rubin L. Injectable fluid silicone therapy: human morbidity and mortality JAMA. 1975; 234(3): 308-309
- Price EA, Schueler H, Perper JA. Massive systemic silicone embolism: a case report and review of literature. Am J Forensic Med Pathol. 2006; 27(2): 97-102.
- Kim CH, Chung DH, Yoo CG, Lee CT, Han SK, Shim YS, et al. A case of acute pneumonitis induced by injection of silicone for colpoplasty. Respiration. 2003; 70(1): 104-6.
- Schmid A, Tzur A, Leshko L, Krieger BP. Silicone embolism syndrome: a case report, review of the literature, and comparison with fat embolism syndrome. Chest. 2005; 127(6): 2276-81.
- Rodriguez MA, Martinez MC, Lopez-Artiguez M, Soria ML, Bernier F, Repetto M. Lung embolism with liquid silicone. J Forensic Sci. 1989; 34(2): 504-10.
- Zamora AC, Collard HR, Barrera L, Mendoza F, Webb WR, Carrillo G. Silicone injection causing acute pneumonitis: a case series. Lung. 2009; 187(4): 241-4.
- Ellenbogen R, Rubin L. Injectable fluid silicone therapy. Human morbidity and mortality. JAMA. 1975; 234(3): 308-9.
- Lai YF, Chao TY, Wong SL. Acute pneumonitis after subcutaneous injections of silicone for augmentation mammaplasty. Chest. 1994; 106(4): 1152-5.
- Celli BR, Kovnat DM. Acute pneumonitis after subcutaneous injections of silicone. N Engl J Med. 1983; 309(14): 856-7.