Reviewed By Allergy, Immunology & Inflammation Assembly
Submitted by
Adam G. Manko MD
Fellow/Clinical Instructor
Division of Pulmonary, Allergy, Critical Care and Sleep Medicine
The Ohio State University Wexner Medical Center
Columbus, OH
Konstantin Shilo, MD
Associate Professor
Department of Pathology
The Ohio State University Wexner Medical Center
Columbus, OH
Jennifer W. McCallister MD
Associate Professor of Clinical Medicine
Division of Pulmonary, Allergy, Critical Care and Sleep Medicine
The Ohio State University Wexner Medical Center
Columbus, OH
Submit your comments to the author(s).
History
A 35 year-old African-American man presented from prison in southwestern Ohio with two weeks of shortness of breath, productive cough with yellow sputum, daily fevers, drenching sweats, unintentional weight loss of 20 pounds, and malaise. He had been incarcerated for 4.5 years, and had not left the prison during that time. He denied tuberculosis exposure or history of a positive purified protein derivative (PPD). He noted several inmates recently diagnosed with pneumonia. It was notable that the outdoor yard at the prison had many pigeons.
His past medical history was significant only for a testicular abscess. His social history was positive for smoking three cigarettes daily since the age of 15. He had no family history of pulmonary disease or malignancy. He did not take any prescription or over the counter medications, and had no known drug allergies.
Physical Exam
Lab
Significant Laboratory data
| White Blood cells | 22.5 k/uL | (4.5-11.0 k/uL) |
| Hemoglobin | 11.9 g/dL | (13.2-17.3 g/dL) |
| Hematocrit | 36.7 % | (39.0-49.0%) |
| Platelets | 565 K/uL | (150-400 K/uL) |
Differential 81.4% neutrophils, 2% band, 5.3% lymphocytes, 8.6% monocytes
| Sodium | 129 mmol/L | (133-143 mmol/L) |
Streptococcus pneumonia urinary antigen – negative
Legionella urinary antigen – negative
Blood cultures – negative
Urine culture – negative
Figures
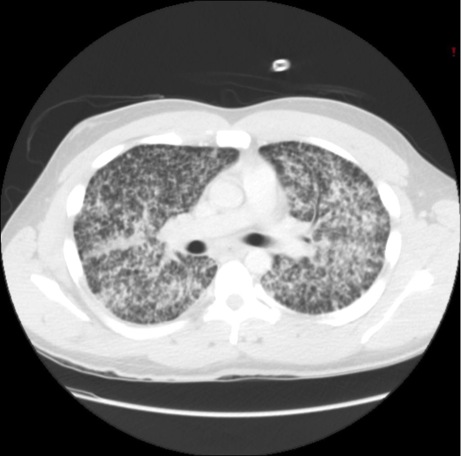
Figure 2: Computed Tomography (CT) of the chest demonstrated diffuse micro-nodular infiltrates throughout both lung fields without associated lymphadenopathy
References
- Chugh IM, Agarwal AK, Arora VK, Shah A. Bilateral miliary pattern in sarcoidosis. The Indian journal of chest diseases & allied sciences 1997; 39: 245-249.
- Curull V, Morell F, Fort J, Espinel E. Dyspnea, fever and miliary pattern. Chest 1985; 88: 285-286.
- Mert A, Ozaras R. Clinical importance of miliary pattern in the chest X-ray of a patient with fever of unknown origin. Internal medicine 2005; 44: 161.
- Davies SF, MD, Knox KS, MD, Sarosi GA, MD. Fungal Infections. Murray and Nadel's textbook of respiratory medicine, 5th ed. Philadelphia, PA.: Saunders; 2010. p. 811-849.
- Furqan M, Butler J. Miliary pattern on chest radiography: TB or not TB? Mayo Clinic proceedings Mayo Clinic 2010; 85: 108.
- Fahim A, Khan MN. An unusual cause of miliary radiographic pattern. BMJ case reports 2011; 2011.
- Paleiron N, Nguyen BV, Commandeur D, Danguy des Deserts M, Rioualen S, Ralec B, Andre M, Ould-Ahmed M, Rousset J. [Miliary X-ray pattern is not always related to tuberculosis]. Medecine et maladies infectieuses 2013; 43: 28-31.
- Katzenstein A-LA, Askin FB. Katzenstein and Askin's surgical pathology of non-neoplastic lung disease. Philadelphia: Elsevier Saunders; 2006.
- Chapman S, Sullivan D. Blastomyces dermatitidis. Mandell, Douglas, and Bennett's principles and practice of infectious diseases, 7th ed. Philadelphia, PA: Churchill Livingstone/Elsevier,; 2010. p. 3319-3332.
- Chapman SW, Dismukes WE, Proia LA, Bradsher RW, Pappas PG, Threlkeld MG, Kauffman CA, Infectious Diseases Society of A. Clinical practice guidelines for the management of blastomycosis: 2008 update by the Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2008; 46: 1801-1812.
- Mongkolrattanothai K, Peev M, Wheat LJ, Marcinak J. Urine antigen detection of blastomycosis in pediatric patients. The Pediatric infectious disease journal 2006; 25: 1076-1078.
- Stockman L, Clark KA, Hunt JM, Roberts GD. Evaluation of commercially available acridinium ester-labeled chemiluminescent DNA probes for culture identification of Blastomyces dermatitidis, Coccidioides immitis, Cryptococcus neoformans, and Histoplasma capsulatum. Journal of clinical microbiology 1993; 31: 845-850.
- Baumgardner DJ, Laundre B. Studies on the molecular ecology of Blastomyces dermatitidis. Mycopathologia 2001; 152: 51-58.