Answer: E
Pulmonary eosinophilia encompasses an array of diverse disorders, all commonly associated with increased numbers of eosinophils in the lungs. Eosinophils are typically found in small amounts in normal lungs (approximately 2%). Pulmonary eosinophilia is characterized by much higher proportions of eosinophils, with greater than 25% being a standard cut-off value.
Acute eosinophilic pneumonia typically presents with acute onset of cough and dyspnea, usually of less than one week in duration. Pleuritic chest pain and myalgias may be present as well. Patients are often febrile, and auscultation of lung fields is usually remarkable for crackles. The average age of onset is 29 years, and 40% of the patients have a history of smoking. Hypoxemia is universally present and this disease frequently progresses to respiratory failure necessitating mechanical ventilation. The disease is steroid responsive and patients rapidly improve with administration of glucocorticoids in modest dosages. This disease may be idiopathic or associated with a wide range of medications, toxins, and occasionally fungal infections.
Chronic eosinophilic pneumonia is a disorder also characterized by marked infiltration of eosinophils in the lungs. Patients typically present with more subacute symptoms including cough, fever, weight loss, wheezing, and night sweats. This disorder frequent occurs in middle-aged women and non-smokers. A diagnosis of asthma usually precedes this diagnosis. Radiographic findings include peripheral infiltrates creating the “photographic negative of pulmonary edema.” This disease is steroid responsive, though it requires a prolonged course of therapy.
Strongyloidiasis is caused by infection with the helminth Stronglyoides Stercoralis. The infection typically begins when larvae in the soil penetrate the skin of bare feet. Transpulmonary migration can eventually result in pulmonary symptoms including cough and dyspnea which paradoxically worsen with corticosteroid therapy. Peripheral eosniophilia is common. Patients may also suffer repeated gram-negative pneumonias cause by bacteria adhering to the larvae.
Churg-Strauss Sydrome (CSS) is a necrotizing, granulomatous vasculitis generally characterized by asthma, sinus disease, and profound peripheral blood eosinophilia. The absolute eosinophil count is generally over 1,500. Radiologic findings vary but typically include patchy infiltrates which may be migratory and fleeting.
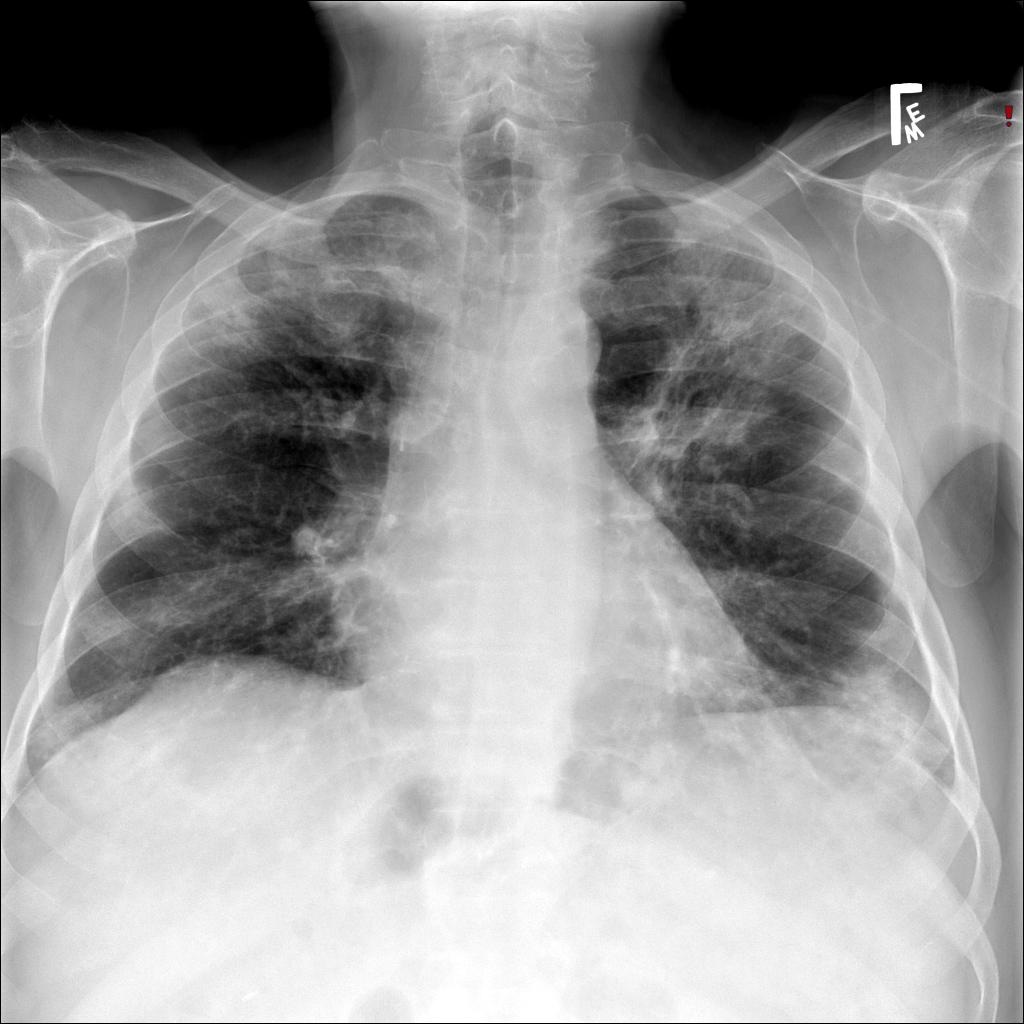
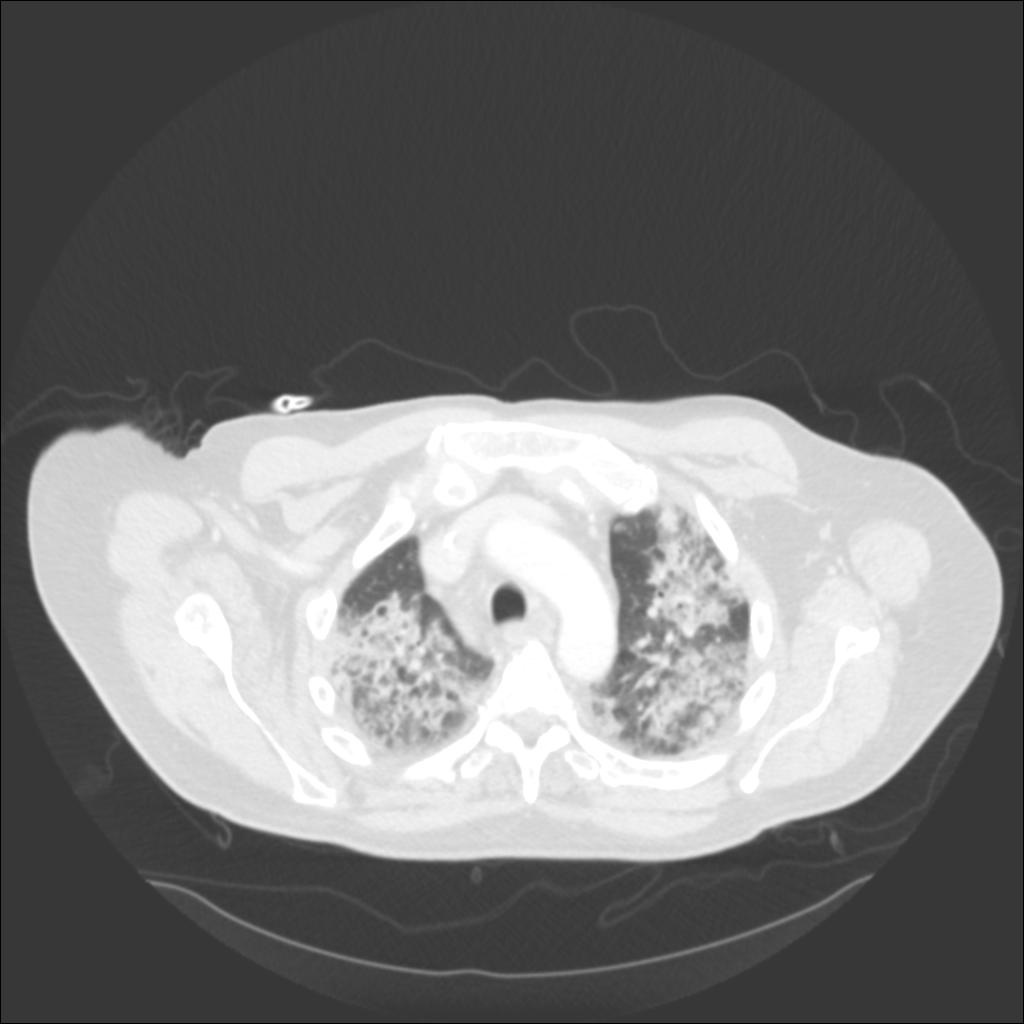
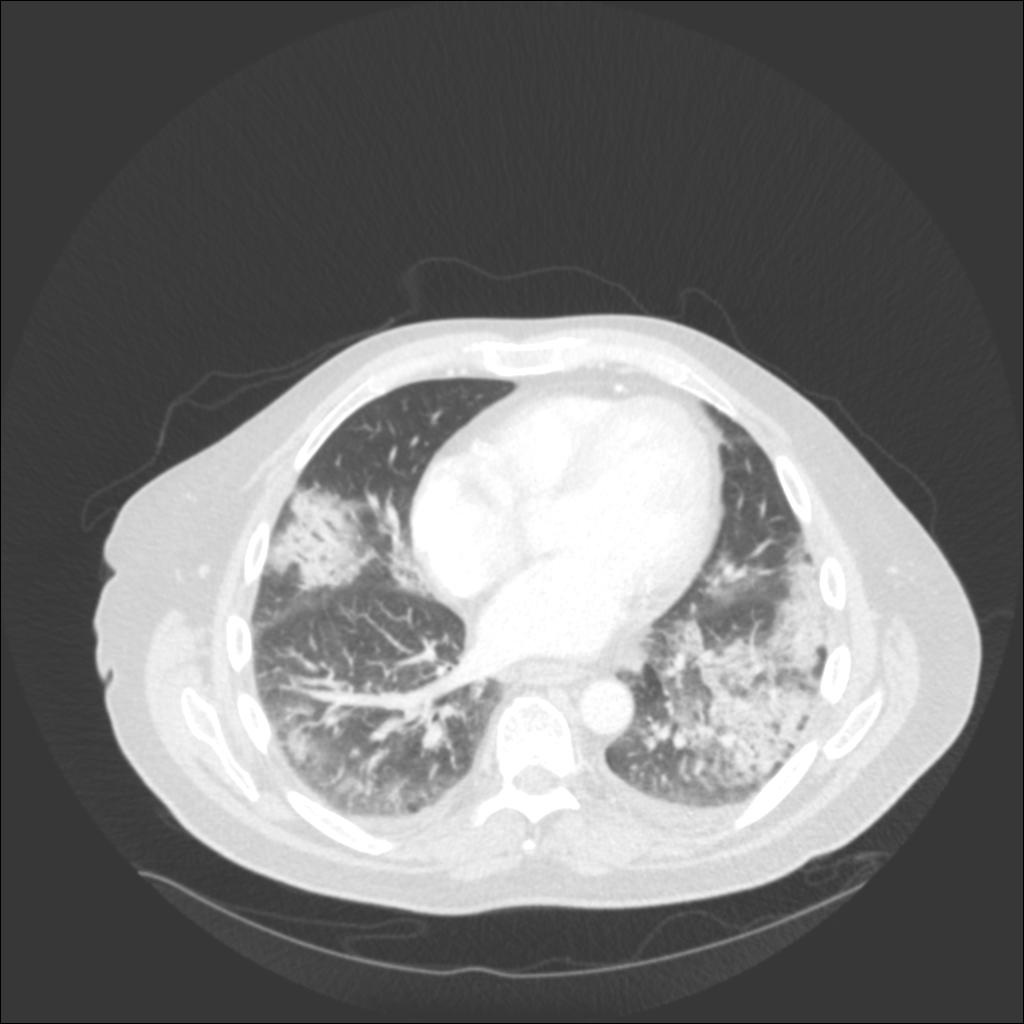
In our patient, the chest radiograph revealed multifocal alveolar infiltrates predominantly in the right upper lobe, left upper lobe, and left lower lobe. Chest CT revealed patchy ground glass and consolidative infiltrates throughout both lungs.
Answer: A
Eosinophilic pneumonia is universally characterized by BAL eosinophilia in patients not currently receiving steroid therapy. Eosinophilia may range anywhere from 20% up to 50% of cells analyzed in the BAL fluid; however, greater than 25% is a generally accepted minimum cut-off value. BAL is therefore very helpful in excluding eosinophilic pneumonia in patients who present with ARDS of unclear etiology.
Fungal immunodiffusion and complement fixation panels would not be diagnostic because the etiology is not likely to be a fungal pathogen. Had the clinical presentation or radiologic findings been consistent with allergic bronchopulmonary aspergillosis (ABPA) or an endemic fungal infection, these labs would be a reasonable approach.
If the bronchoalveolar lavage results were unrevealing, consideration would be given to obtaining tissue via transbronchial or surgical lung biopsy. Pathologic findings in acute eosinophilic pneumonia commonly include diffuse alveolar damage, interstitial and alveolar eosinophil infiltration, and lymphocyte infiltration. However, neither would be the preferred initial approach as BAL is universally suggestive of the diagnosis in patients not already treated with corticosteroids.
Small bilateral pleural effusions are common in acute eosinophilic pneumonia. Effusions are typically exudative and may reveal eosinophils, however, results are generally non-specific. Thoracentesis would be unhelpful in this scenario given the lack of pleural effusion on imaging.
Bronchoscopy with BAL was subsequently performed in our patient. The cell count/differential was significant for 27% eosinophils. Initial gram stain of BAL fluid was negative and bacterial, fungal, and acid fast cultures remained negative.
Answer: E
Although peripheral eosinophilia is common in chronic eosinophilic pneumonia (CEP), it is rarely found at onset of idiopathic AEP. Rash is also uncommon with idiopathic AEP. Pulmonary eosinophilia is well known to be a complication of many medications. Drug-associated pulmonary eosinophilia has been associated with a wide range of disease severity, from asymptomatic to eosinophilic pneumonia with respiratory failure. Peripheral blood eosinophilias, as well as rash, are commonly associated with drug-related eosinophilic pneumonia as opposed to the idiopathic form of the disease. Biopsy of skin lesions will frequently demonstrate perivascular infiltration of lymphocytes and eosinophils.4
Answer: B
Several classes of drugs have been associated with pulmonary eosinophilia. These include antimicrobials (daptomycin, minocycline) anti-epileptics, and NSAIDs. Case reports have also described mexilitine-induced AEP. 4 SSRIs, particularly sertraline, have been associated with AEP, but this is less common. Other causes of AEP include environmental exposures like firework smoke, gasoline tank cleaning, cave exploration, and woodpile moving. Cigarette smoke is also a potential trigger, especially in new-onset smokers. Fungal infections can also trigger AEP, namely coccidiomycosis.
Several cases of daptomycin-induced AEP have been reported in the literature.2,5 One case series described three patients with osteomyelitis or prosthetic joint infections treated with daptomycin. In two of the patients, signs and symptoms resolved simply with the removal of daptomycin; the third required a short course of corticosteroids.5
Albuterol, hydrochlorothiazide, and lisinopril are not known to be associated with AEP.
Answer: A
The first step in treatment of drug-associated eosinophilic pneumonia is the removal of the suspected offending agent. If the patient’s condition fails to improve with the removal of the offending agent, treatment with corticosteroids is then warranted. Patients with eosinophilic pneumonia are uniformly responsive to corticosteroid therapy, and the response is often dramatic.
A case series described two patients who were both in their eighties and were being treated with daptomycin for infected prosthetic joints. Both cases resolved initially after stopping daptomycin and starting corticosteroids, but symptoms recurred after steroids were discontinued necessitating chronic low-dose corticosteroid therapy.3
Broad-spectrum antibiotics cannot be used for treatment because the condition is not caused by a bacterial infection and in fact, antibiotics are often the cause of this condition. Pulmonary rehabilitation is a long-term therapy and would have no benefit for AEP in the acute setting. Continuing the offending agent would be inappropriate and would lead to progression of disease