Reviewed By Allergy, Immunology & Inflammation Assembly
Submitted by
Daniel J. Schneider MD, PhD
Clinical Lecturer
Department of Internal Medicine
University of Michigan Hospitals
Ann Arbor, MI
Submit your comments to the author(s).
History
Learning objectives:
- Review the differential diagnosis for severe asthma with eosinophilia and pulmonary infiltrates.
- Understand the historical, laboratory, imaging, and histopathologic manifestations of conditions that ‘mimick’ severe asthma.
- Explore novel biologic treatment options for management of eosinophilia.
22 year old male with a history of rhinorrhea and nasal congestion as a child presented with shortness of breath and cough. He is a lifelong non-smoker and has no history of respiratory symptoms until 1 year prior to presentation. In the span of the preceding year, he experienced 5 episodes of chest congestion, productive cough, wheezing, and shortness of breath which were treated successfully, albeit temporarily with varying doses of prednisone. He lives in Michigan and has not traveled outside of the state recently. At this time he was also diagnosed with nasal polyps. Initial maintenance treatments for his asthma included budesonide/formoterol 160/4.5 mcg twice daily, montelukast 10mg daily, prednisone 20mg daily, and cetirizine 10mg daily. Based on an elevated IgE he was eventually started on omalizumab without adequate control of his symptoms.
Pertinent laboratory evaluation performed at the time included myeloperoxidase and proteinase 3 ANCA which were negative, absolute eosinophil count and total IgE were elevated at 4.6k/μL and 512 kU/L, respectively. Bronchoscopy was performed which showed 68% eosinophils on BAL cell differential and no evidence of infection. He was started on benralizumab given his peripheral and airway eosinophilia despite 20mg of prednisone.
Despite this initiation, he developed generalized abdominal pain, nausea, vomiting, diarrhea, fevers at home (38.9 °C), lymphadenopathy, and worsening shortness of breath which lead to a hospital admission. It was noted on interview that he had been unable to refill his prednisone 1 week prior to the admission.
Physical Exam
Pertinent physical exam findings:
Temp: 37.2 °C, BP 148/90, HR: 116, Resp: 20, SPO2: 99% RA
Rales throughout all lung fields, greatest at right base. Abdomen tender to palpation in right upper quadrant.
Outpatient pulmonary function testing:
Oximetry at rest on room air: 94%
| Pre-bronchodilator | ||
| Absolute | % Predicted | |
| FVC | 4.73 L | 80% |
| FEV1 | 2.89 L | 62% |
| FEV1:FVC | 61% | 77% |
Laboratory evaluation at admission
Basic metabolic panel normal including Cr 0.83
WBC 14.2 K/μL, Hgb 13.2 g/dL, Plt 479 K/μL, Abs eos 0.4 K/μL
ESR 68, CRP 9.8 (0.0 - 0.6), ANA negative, repeat ANCA negative
IgE 4763 kU/L, Aspergillus IgE < 0.35 kU/L
| Urinalysis |
|
Protein | Negative | |
| Color | Yellow |
|
Glucose | Negative |
| Appearance | Normal |
|
Ketones | Negative |
| Specific Gravity | 1.022 |
|
Urobilinogen | Negative |
| pH | 7.0 |
|
Bilirubin | Negative |
| Leukocyte esterase | Negative |
|
Blood | Negative |
| Nitrite | Negative | RBC/HPF | Negative |
Stool ova and parasite testing, stool viral PCR panel, and strongyloides antibody were all negative.
Imaging performed during admission
CT scan of the abdomen and pelvis: notable for wall thickening and mucosal enhancement of the duodenum and proximal jejunum consistent with enteritis that could be infectious or inflammatory in nature. Small amount of surrounding free fluid.
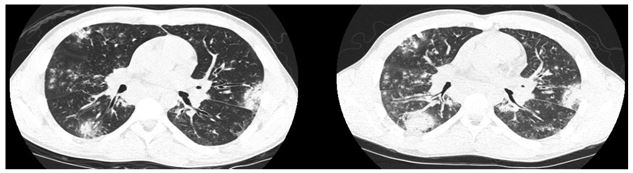
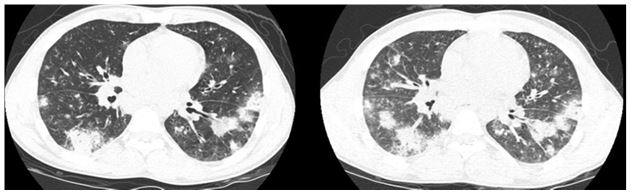
High resolution CT of the chest: (representative image shown; inspiratory (left) expiratory (right))
Transthoracic echocardiogram: Normal LV/RV function.
Procedures and associated histology findings during admission:
Endoscopy and push enteroscopy: gastric, duodenal, and jejunal biopsies were taken. All biopsies were negative for eosinophilic infiltrates or viral inclusions.
Repeat bronchoscopy: showed a decline in airway eosinophils to 2% and BAL cultures were again negative. Transbronchial biopsies showed only normal and exfoliated respiratory epithelium. Notably, the patient had 1 dose of prednisone 20mg the day prior to repeat bronchoscopy.
Bone marrow biopsy: normocellular aspirate, trilineage hematopoiesis, and peripheral eosinophilia consistent with reactive eosinophilia. (serum absolute eosinophils 3.9 K/μL at time of biopsy)
Flow cytometry was normal
Fluorescent in situ hybridization and showed a normal male karyotype;
notable absence of FIP1L1/PDGFRA gene fusion, rearrangements, or mutations within of PDGFRA, PDGFRB, FGFR1 or JAK2 genes.
Clonal rearrangement in T cell receptor β (TRB) was detected
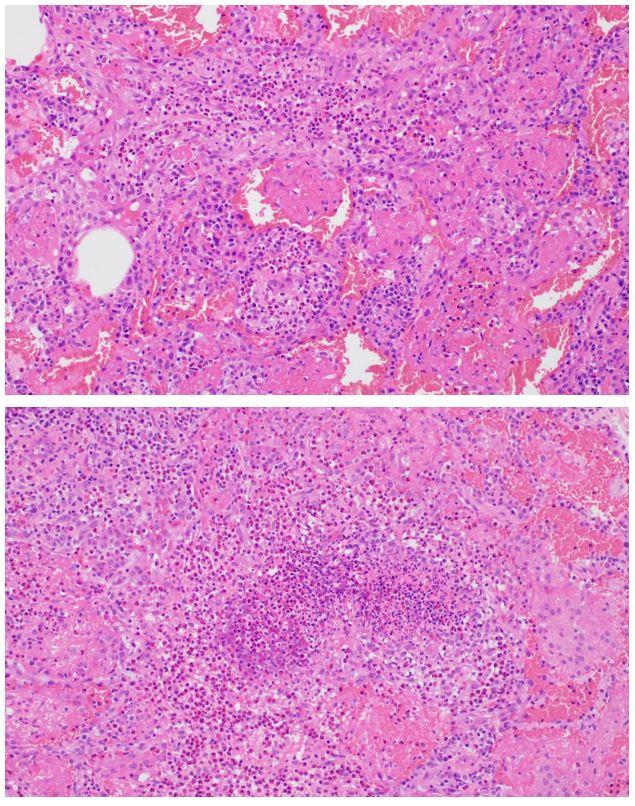
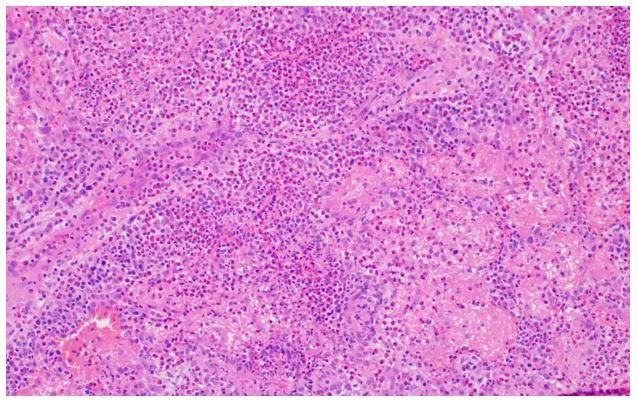
Video-assisted thorascopic surgery wedge biopsy of the right lower lobe: – H&E sections (3):
References
- Churg A, Brallas M, Cronin SR, Churg J. Formes frustes of Churg-Strauss syndrome. Chest 1995; 108:320.
- Comarmond C, Pagnoux C, Khellaf M, et al. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss): clinical characteristics and long-term followup of the 383 patients enrolled in the French Vasculitis Study Group cohort. Arthritis Rheum 2013; 65:270.
- Cottin V, Bel E, Bottero P, et al. Revisiting the systemic vasculitis in eosinophilic granulomatosis with polyangiitis (Churg-Strauss): A study of 157 patients by the Groupe d'Etudes et de Recherche sur les Maladies Orphelines Pulmonaires and the European Respiratory Society Taskforce on eosinophilic granulomatosis with polyangiitis (Churg-Strauss). Autoimmun Rev 2017; 16:1.
- Gioffredi A, Maritati F, Oliva E, Buzio C. Eosinophilic Granulomatosis with Polyangiitis: An Overview. Front Immunol. 2014; 5: 549.
- Ortega HG, Liu MC, Pavord ID, Brusselle GG, FitzGerald JM, Chetta A, Humbert M, Katz LE, Keene ON, Yancey SW, Chanez P; MENSA Investigators. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014 Sep 25;371(13):1198-207. doi: 10.1056/NEJMoa1403290.
- Sablé-Fourtassou R, Cohen P, Mahr A, Pagnoux C, Mouthon L, Jayne D, Blockmans D, Cordier JF, Delaval P, Puechal X, Lauque D, Viallard JF, Zoulim A, Guillevin L; French Vasculitis Study Group. Antineutrophil cytoplasmic antibodies and the Churg-Strauss syndrome. Ann Intern Med. 2005 Nov 1;143(9):632-8.
- Sinico RA, Di Toma L, Maggiore U, Bottero P, Radice A, Tosoni C, et al. Prevalence and clinical significance of antineutrophil cytoplasmic antibodies in Churg-Strauss syndrome. Arthritis Rheum (2005) 52(9):2926–35.10.1002/art.21250
- Wechsler ME, Akuthota P, Jayne D, Khoury P, Klion A, Langford CA, Merkel PA, Moosig F, Specks U, Cid MC, Luqmani R, Brown J, Mallett S, Philipson R, Yancey SW, Steinfeld J, Weller PF, Gleich GJ; EGPA Mepolizumab Study Team. Mepolizumab or Placebo for Eosinophilic Granulomatosis with Polyangiitis. N Engl J Med. 2017 May 18;376(20):1921-1932. doi: 10.1056/NEJMoa1702079.