Reviewed By Allergy, Immunology & Inflammation Assembly
Submitted by
Navjeet Uppal, MD
Division of Respiratory Medicine
Department of Medicine
University of Toronto
Toronto
Susan M Tarlo MB BS
Division of Respiratory Medicine
Department of Medicine
University of Toronto
Toronto
Submit your comments to the author(s).
History
A 44 year old woman, currently working in a bakery, presents with a 1 year history of asthma and allergic rhinitis symptoms, including episodic cough, wheeze, shortness of breath and chest tightness with itchy red watery eyes and a stuffy, runny, itchy nose. These symptoms become worse within 1-2 hours of starting work each day, and worsen throughout the work week. She especially finds red bran to worsen her symptoms almost immediately on exposure. She notices an improvement within 1-2 hours outside of being at her workplace. She has been working in the bakery for 13 years, and for the last 10 years has been a "pre-scaler", weighing components, while wearing a paper mask. The line that she has worked on for the last 2 years is dustier than other areas.
Her past medical history is significant for seasonal allergic rhinitis in the summer months since childhood. She is a lifelong non-smoker. Her family history is significant for asthma in her mother and brother. She currently uses an inhaled steroid-long acting bronchodilator (ICS-LABA) daily, and inhaled short-acting bronchodilator (SABA) as needed, generally up to 4 times a day at work with relief.
Physical Exam
Her physical examination is normal.
Lab
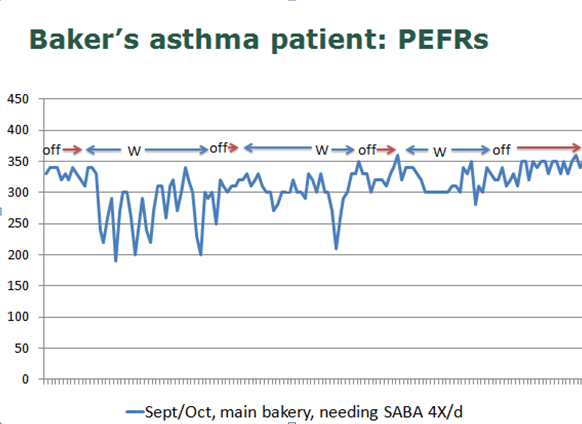
Her chest x-ray is also normal. Spirometry testing shows FEV1/FVC 0.62 (within 24 hours of work), FEV1 1.9L (60% predicted), and post-bronchodilator, the FEV1 increases to 2.2L (300cc, 16%). One year earlier, after 2 months off work, her FEV1 was 2.3L. Skin prick testing was positive to grass (3+), a slurry of workplace flour (3+), wheat germ (3+), and red bran (2+). Her home peak expiratory flow readings ranged between 270 and 340, with lower readings on workdays (figure 1).
Diagnosis and Management
A diagnosis of occupational asthma from wheat (including wheat germ and bran) was made. She was transferred to a muffin packing area where flour exposure was minimal, if any, and was followed with further peak flow monitoring and spirometry: she has since remained well with no symptoms and requiring no medications.
Spirometry testing shows FEV1/FVC 0.62 (within 24 hours of work), FEV1 1.9L (60% predicted), and post-bronchodilator, the FEV1 increases to 2.2L (300cc, 16%). One year earlier, after 2 months off work, her FEV1 was 2.3L. Skin prick testing was positive to grass (3+), a slurry of workplace flour (3+), wheat germ (3+), and red bran (2+). Her home peak expiratory flow readings ranged between 270 and 340, with lower readings on workdays (figure 1).
Figures
References
- Baatjies R, Meijster T, Heederik D, Sander I, Jeebhay MF. Effectiveness of interventions to reduce flour dust exposures in supermarket bakeries in South Africa. Occup Environ Med 2014;71:811-8.
- Baatjies R, Meijster T, Heederik D, Jeebhay MF. Exposure-response relationships for inhalant wheat allergen exposure and asthma. Occup Environ Med 2015;72:200–207.
- Gautrin D, Ghezzo H, Infante-Rivard C, Malo JL. Incidence and determinants of IgE-mediated sensitization in apprentices: a prospective study. Am J Respir Crit Care Med 2000;162:1222-8.
- Heederik D, Henneberger PK, Redlich CA. Primary prevention: exposure reduction, skin exposure and respiratory protection. Eur Respir Rev 2012;21:112-24.
- Malo JL, Chan-Yeung M. Agents causing occupational asthma. J Allergy Clin Immunol 2009;123(3):545-50.
- Tarlo SM, Balmes J, Balkissoon R, et al. Diagnosis and management of work-related asthma: American College Of Chest Physicians Consensus Statement. Chest 2008; 134:Suppl:1S-41S. [Erratum, Chest 2008; 134:892.]
- Tarlo SM, Lemiere C. Occupational asthma. NEJM 2014;370(7):640-9.
- Tarlo SM, Liss GM. Prevention of occupational asthma. Curr Allergy Asthma Rep 2010;10:278-86.