One year after I started as a newly independent junior faculty member, I became Medical Director of Respiratory Therapy. At first, I welcomed the job and was flattered by the title. Despite my lack of formal training in management or leadership skills I assumed that I was ready for the job. After all, I had spent years learning how to be a leader, honing my skills in data analysis and problem solving. I never thought about the fact that up until this time my training had solely occurred in patient-care venues, e.g. the ICU, the OR, and ER, where physicians acted as leaders in a chain of command model. It never occurred to me that my physician-scientist training might actually hamper my efforts to supervise a not entirely functional group of 12 respiratory therapists.
In fact, I soon discovered that the skills which worked so well for me in the clinical setting made me seem autocratic and sometimes clumsy as a manager. I was taught to be an autonomous decision maker - a team leader, not a team builder. Through my training, I learned a vertical approach to problem solving. I made decisions based on logic and evidence. After reaching a conclusion based on the available facts, there was no need to gather opinions prior to making a decision. I expected to lead not by building consensus but by having others simply follow. As it turns out, this was incredibly naive given the deep-rooted conflicts that existed between members of the department. Instead, I had to rely on native social skills and common sense in dealing with the distrust and low morale that had accumulated over the years. But even then, I needed to learn the difference between being well liked and respected. Conflict resolution was only the beginning of our problems. What about performance review? Budget analysis?
Saying that physicians are poorly trained to be managers is not new. Articles complaining about the lack of effective physician managers go back at least 10-15 years. Not surprisingly, they also parallel the gradual waning influence of the medical profession in healthcare. Hospitals used to be run by physicians. As medical centers have grown larger, more complex, and profit-oriented, a physician-run hospital has become the exception rather than the norm. Although physicians are loosely organized into their own hierarchies, they are typically divided along lines of expertise with specialists and subspecialists competing among themselves for resources. Except for positions such as chief medical officer, physicians have become largely relegated to middle management. Their authority is further splintered by division along patient care lines. For instance, it is not unusual to have two chiefs of medicine to manage the in-patient and out-patient services.
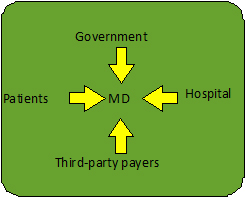
As a result, a dramatic shift in power has occurred mainly at the strategic decision level. By giving up or relegating positions of authority to business trainees with minimal patient care experience or to physicians with minimal management training, the medical profession has further exacerbated its loss of influence. Given how poorly we are integrated into hospital organizational infrastructure, is it any wonder that many of us feel like glorified assembly line workers? Although the physician remains accountable for patient care, it is incredible how little power we actually wield these days. On one side, we are buffeted by administrators, nurses, pharmacists, billers and coders. Third party payers and government dictate clinical practice through their constant second-guessing of physician decision making and formulation of performance guidelines. Even patients no longer regard physicians with the same respect as consumer magazines preach a patient-centric approach to healthcare based on knowledge gleaned from self-help gurus and the Internet.
Team building, organizational performance, and quality improvement are inescapable facts of everyday medical life, be it academic or practice based. Unfortunately, current medical training largely ignores critical knowledge and skills that a physician needs to survive let alone thrive in healthcare these days. ACGME standards are hardly state of the art. They reflect the minimum of medical knowledge needed to practice. And yet many programs are focused on accomplishing just that - the bare minimum. Another relatively overlooked reason contributing to why medical training programs have failed to keep up with fundamental changes in healthcare is the fact that this training occurs largely in academic institutions whose economic viability depends on indirect costs provided by NIH grants. Not surprisingly, this has led to an insular, research-based culture in which administrative jobs are viewed as trivial distractions and prestige is directly measured in terms of publications and grants. Furthermore, while NIH institutional grants support postdoctoral training, the funds are typically used to train physician-scientists only in the narrowest sense. The fact that poorly paid postdoctoral fellows are often viewed as intellectually vital yet cheap labor for the research enterprise has meant even less incentive to change the system.
However, we must rethink our definition of what a physician-leader is. Besides the loss of professional sovereignty, we must also consider economic reality. Given declining NIH budgets and expensive government bail-outs, it does not matter whether you are an academic chief or head of a private practice group, leadership now demands scientifically literate and financially savvy physicians who can work effectively with hospital administrators to strategically manage increasingly limited resources. Furthermore, not everyone can be an R01-funded physician-scientist. Just compare the number of postdoctoral fellowships to the number of funded K awards versus the number of R01s and do the math. And yet the system does little to help those who do not stay in research, leaving a sizable number of highly trained physicians with varying degrees of scientific prowess who have few options other than to go into practice. What a waste! True, some segue into pharma or biotech. Others manage to work their way up the hospital organizational ladder or find their way into MBA programs or government fellowships. But why not proactively train leaders who are capable of bridging the often hostile gap between physician and organizational hierarchies in order to create an environment in which healthcare providers and patients thrive? We need physicians who can advocate for how hospitals invest their “profits”, who can work with information technology to develop tools designed to enhance instead of impede productivity, and who can develop meaningful outcome measures that are realistic measures of quality.
I am not arguing for elimination of scientific training. Such training provides us with a unique perspective not matched by ancillary healthcare providers in that we can keep up with translational science and evaluate healthcare trends. The ability to critically analyze data, create hypotheses, and come up with conclusions as well as alternative viewpoints can be a powerful tool when used appropriately. Furthermore, pulmonary, critical care, and sleep physicians are uniquely suited to become physician-executives. Our ICU training demands that we think broadly and process multiple data streams. Instead of viewing positions such RT, ICU, PFT laboratory directorships as unimportant, we should appreciate them as unique opportunities to gain valuable real-world administrative experience. However, it is not enough to think that these skills can be learned ad hoc or that they cannot be improved upon with formal training. Instead of a one-size fits all approach to fellowship training, why not develop CMS-NIH funded programs aimed at training physician-leaders who understand what it takes to efficiently deliver quality healthcare in a cost-efficient manner. These skills go beyond the business world. Knowing how to hire good help and develop an engaged, productive team is critical whether you are running a respiratory therapy department, trying to understand the role of stem cells in lung injury, or seeing four patients an hour in a clinic. Employee turnover is just as devastating to a small laboratory as it is to a busy clinic.
We cannot be too busy running our labs and taking care of patients to think of these tasks as “other people’s jobs.” Healthcare is not a commodity. Physicians and patients are not widgets. We, more than anyone else, understand that high-quality care and lower costs are not mutually exclusive, and what must be done to achieve those goals. Ultimately, it is the physician who shoulders the responsibility for the life of the patient and thus only s/he can truly understand what that means and what it takes to protect that life from the financial bottom line.



